Broward Florida Qualifying Event Notice Information for Employer to Plan Administrator: Introduction: The Broward Florida Qualifying Event Notice is a crucial document that employers must provide to their Plan Administrator (also known as the Health Insurance Provider) to ensure compliance with the state regulations and eligibility requirements. This detailed description will outline the essential information contained within this notice and explain the different types of qualifying events that can occur in Broward Florida. Key elements of Broward Florida Qualifying Event Notice Information: 1. Purpose: The primary purpose of the Broward Florida Qualifying Event Notice is to inform the Plan Administrator about any qualifying events that have taken place within an employee's life. These qualifying events may have an impact on the employee's health insurance coverage, such as gaining or losing eligibility or experiencing a change in coverage options. 2. Timeliness: Employers must ensure that the Qualifying Event Notice is provided to the Plan Administrator within the specified time frame set by Broward Florida regulations. Failure to meet the designated timeline may result in penalties or non-compliance with state requirements. 3. Employee Information: The Qualifying Event Notice must include detailed information about the employee experiencing the qualifying event. This should include the employee's name, date of birth, social security number, contact information, and employment details. 4. Qualifying Event Types: Broward Florida recognizes several types of qualifying events that could necessitate the submission of the Qualifying Event Notice, including but not limited to: a. Marriage or Divorce: — Description: This event occurs when an employee gets married or divorces their spouse. — Impact: It may result in changes to the employee's coverage options, as they may need to add or remove their spouse from the plan. b. Birth, Adoption, or Placement for Adoption: — Description: This event occurs when an employee and their spouse experience the birth of a child, adopt a child, or place a child for adoption. — Impact: It may require the employee to update their coverage to include the newborn or adopted child. c. Loss of Dependent Status: — Description: This event happens when an employee's dependent child no longer qualifies for coverage under the plan (e.g., turning 26 years old). — Impact: It may result in the removal of the dependent child from the employee's insurance plan. d. Termination or Commencement of Employment: — Description: This event occurs when an employee terminates or begins a new employment. — Impact: It may require the employee to switch their insurance plan or enroll in a new plan offered by the employer. 5. Documentation Requirements: The Qualifying Event Notice must be supported by appropriate documentation related to the qualifying event, such as marriage certificates, birth certificates, adoption papers, court orders, termination letters, or employment offer letters. These documents serve as evidence for the occurrence of the qualifying event. Conclusion: The Broward Florida Qualifying Event Notice Information for Employer to Plan Administrator plays a vital role in ensuring that the Plan Administrator has accurate and timely information regarding qualifying events. Employers must be aware of the different types of qualifying events and provide all necessary documentation to comply with state regulations effectively. By adhering to the requirements, employers can ensure the uninterrupted provision of health insurance coverage to their employees.
Broward Florida Qualifying Event Notice Information for Employer to Plan Administrator
Description
How to fill out Broward Florida Qualifying Event Notice Information For Employer To Plan Administrator?
How much time does it usually take you to draw up a legal document? Since every state has its laws and regulations for every life scenario, locating a Broward Qualifying Event Notice Information for Employer to Plan Administrator meeting all regional requirements can be exhausting, and ordering it from a professional attorney is often pricey. Many online services offer the most popular state-specific templates for download, but using the US Legal Forms library is most advantegeous.
US Legal Forms is the most extensive online collection of templates, collected by states and areas of use. Apart from the Broward Qualifying Event Notice Information for Employer to Plan Administrator, here you can get any specific form to run your business or personal deeds, complying with your regional requirements. Experts verify all samples for their actuality, so you can be certain to prepare your paperwork properly.
Using the service is pretty easy. If you already have an account on the platform and your subscription is valid, you only need to log in, pick the needed form, and download it. You can retain the file in your profile at any moment later on. Otherwise, if you are new to the platform, there will be a few more actions to complete before you get your Broward Qualifying Event Notice Information for Employer to Plan Administrator:
- Check the content of the page you’re on.
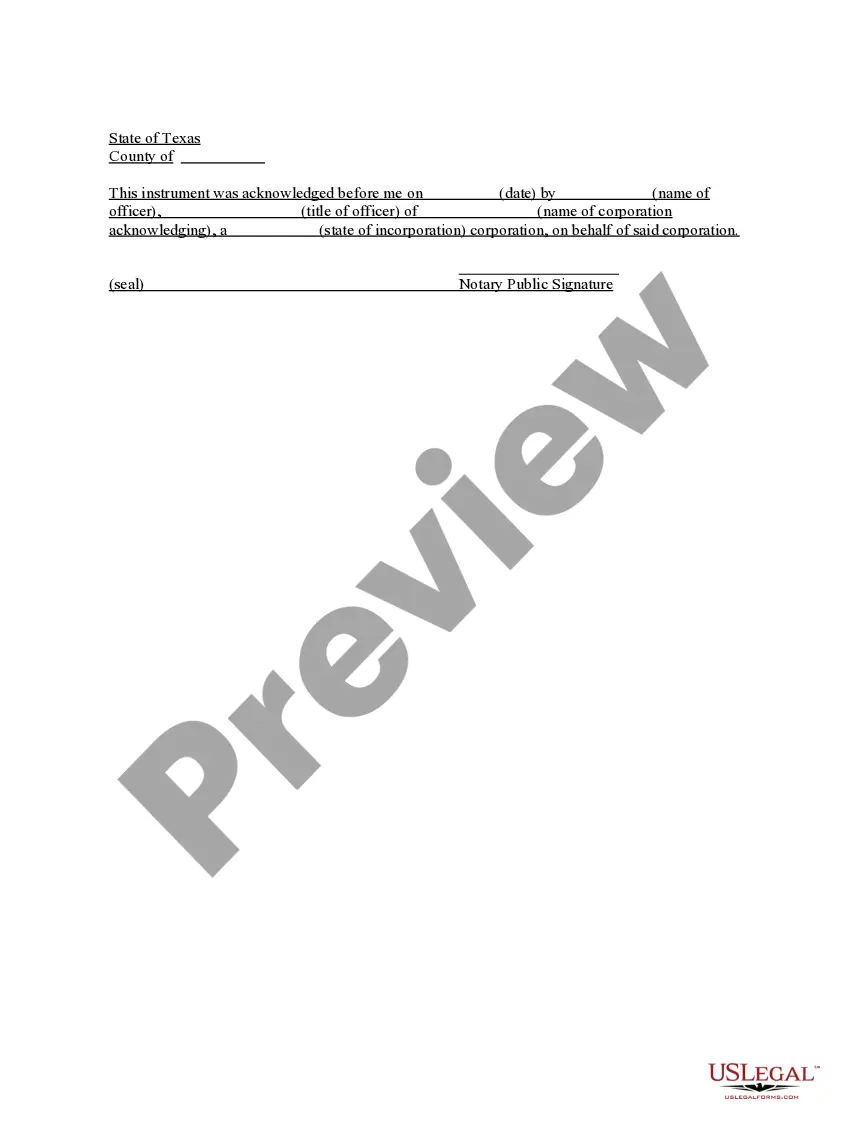
- Read the description of the template or Preview it (if available).
- Search for another form using the corresponding option in the header.
- Click Buy Now when you’re certain in the selected file.
- Select the subscription plan that suits you most.
- Register for an account on the platform or log in to proceed to payment options.
- Make a payment via PalPal or with your credit card.
- Switch the file format if needed.
- Click Download to save the Broward Qualifying Event Notice Information for Employer to Plan Administrator.
- Print the sample or use any preferred online editor to fill it out electronically.
No matter how many times you need to use the acquired template, you can find all the samples you’ve ever downloaded in your profile by opening the My Forms tab. Try it out!