Contra Costa California Qualifying Event Notice Information for Employer to Plan Administrator is a crucial communication that needs to be provided to the plan administrator in compliance with the state regulations. This notice ensures that employers are aware of various qualifying events that may affect an employee's eligibility for benefits or necessitate changes to their existing coverage. The following are different types of Contra Costa California Qualifying Event Notice Information that an employer should be aware of: 1. Birth or adoption: If an employee or their spouse/domestic partner has a child, the employer must be notified within 30 days of the event. This allows the plan administrator to consider adding the newborn or adopted child to the health insurance plan or any other applicable coverage. 2. Loss of dependent status: In case an employee's dependent child no longer qualifies for coverage due to age limits or other eligibility criteria, the employer should be notified as soon as possible. This allows the plan administrator to adjust the coverage accordingly. 3. Marriage or divorce: If an employee gets married or goes through a divorce, it is essential to inform the employer promptly. This event may lead to changes in benefits, including health insurance coverage, spousal support, or beneficiary designations. 4. Loss of coverage: If an employee or their dependents lose coverage due to a reduction in work hours, termination of employment, or any other reason, the employer needs to be notified. This helps the plan administrator determine if the affected individuals are eligible for COBRA continuation coverage or any other alternatives. 5. Change in employment status: Any change in employment status, such as going from full-time to part-time, can impact an employee's eligibility for certain benefits. It is vital to inform the employer promptly to ensure accurate reporting and appropriate adjustments. 6. Change in residence: In the event of an employee changing their residence, the employer should be notified to ensure that the plan administrator can update the employee's address and contact information. This helps in delivering important communications and ensures uninterrupted coverage. 7. Loss of Medicare or Medicaid eligibility: If an employee or their dependents lose eligibility for Medicare or Medicaid, it is crucial to inform the employer. The plan administrator needs to review the circumstances and determine if any adjustments to the coverage are required. Accurate and timely reporting of qualifying events to the employer by employees ensures that the plan administrator can administer the benefits program efficiently and avoids any potential non-compliance issues. Employers should provide clear guidelines and communication channels to employees to facilitate the reporting process effectively. By adhering to the Contra Costa California Qualifying Event Notice Information requirements and promptly notifying the plan administrator of any qualifying events, employers can maintain compliance with state regulations, promote employee welfare, and ensure the efficient utilization of the benefits program.
Contra Costa California Qualifying Event Notice Information for Employer to Plan Administrator
Description
How to fill out Contra Costa California Qualifying Event Notice Information For Employer To Plan Administrator?
Preparing papers for the business or individual needs is always a big responsibility. When creating a contract, a public service request, or a power of attorney, it's crucial to consider all federal and state regulations of the specific region. Nevertheless, small counties and even cities also have legislative procedures that you need to consider. All these aspects make it tense and time-consuming to create Contra Costa Qualifying Event Notice Information for Employer to Plan Administrator without expert help.
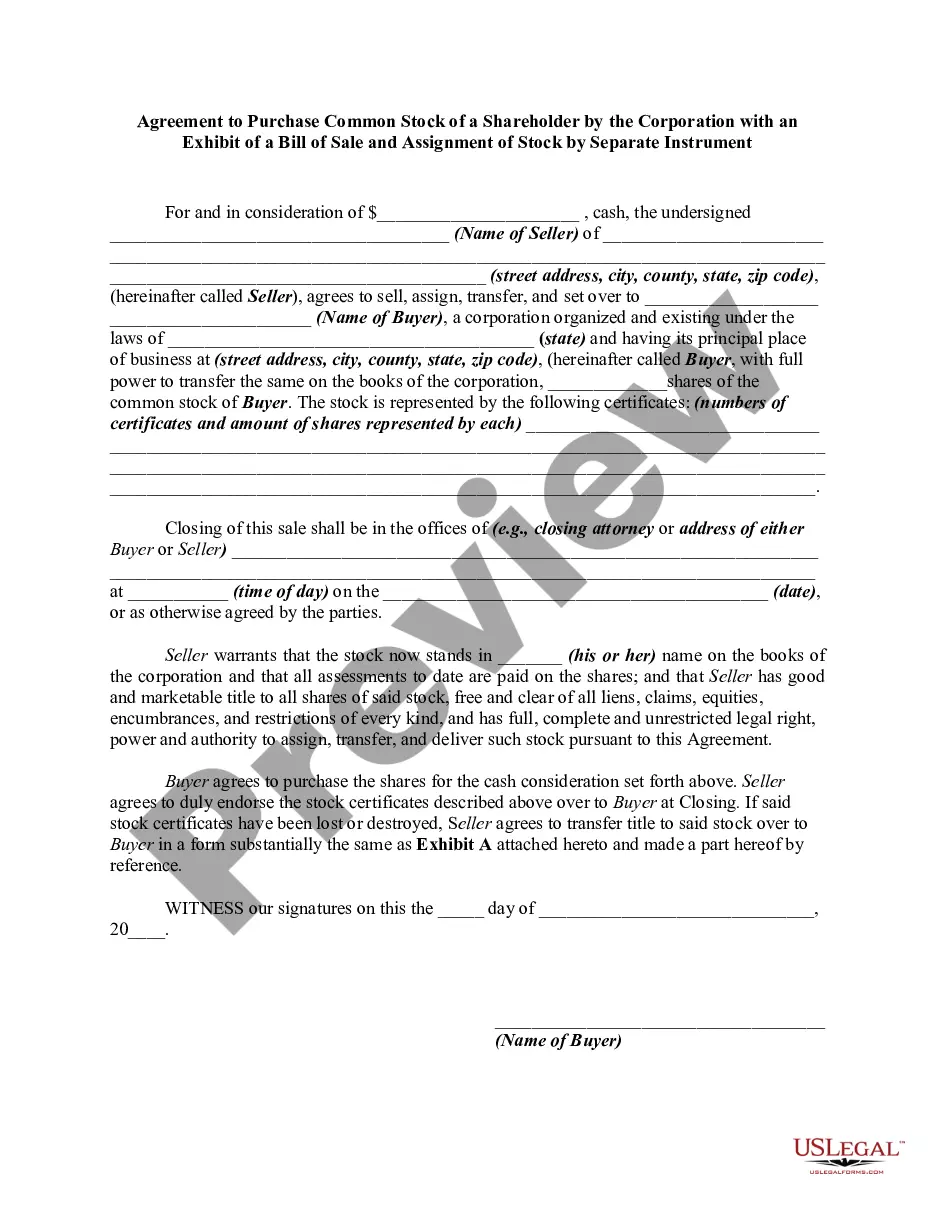
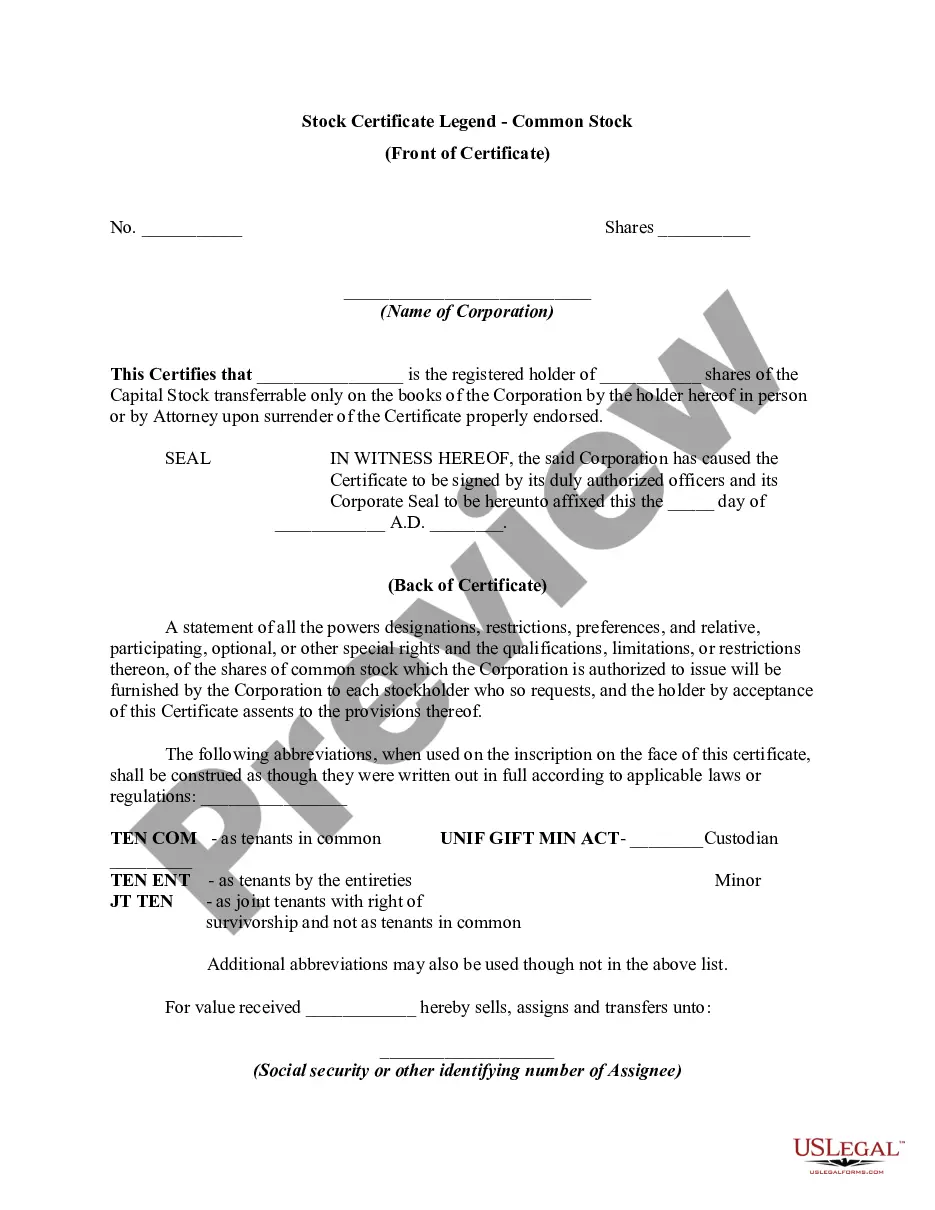
It's easy to avoid spending money on attorneys drafting your paperwork and create a legally valid Contra Costa Qualifying Event Notice Information for Employer to Plan Administrator on your own, using the US Legal Forms online library. It is the greatest online collection of state-specific legal templates that are professionally verified, so you can be sure of their validity when choosing a sample for your county. Earlier subscribed users only need to log in to their accounts to download the required document.
If you still don't have a subscription, follow the step-by-step guide below to get the Contra Costa Qualifying Event Notice Information for Employer to Plan Administrator:
- Look through the page you've opened and verify if it has the sample you need.
- To do so, use the form description and preview if these options are presented.
- To locate the one that suits your requirements, utilize the search tab in the page header.
- Double-check that the sample complies with juridical criteria and click Buy Now.
- Pick the subscription plan, then log in or register for an account with the US Legal Forms.
- Use your credit card or PayPal account to pay for your subscription.
- Download the selected file in the preferred format, print it, or complete it electronically.
The great thing about the US Legal Forms library is that all the paperwork you've ever purchased never gets lost - you can access it in your profile within the My Forms tab at any time. Join the platform and quickly obtain verified legal forms for any use case with just a couple of clicks!