Maricopa, Arizona Qualifying Event Notice Information for Employer to Plan Administrator: A Comprehensive Overview At times, employees in Maricopa, Arizona may experience certain life events that could potentially impact their eligibility for benefits offered by their employer. In such cases, federal regulations require employers to provide a Qualifying Event Notice (MEN) to their Plan Administrator. This detailed description aims to provide essential information regarding Lens in Maricopa, Arizona, including the various types that employers may encounter. What is a Qualifying Event Notice (MEN)? An MEN are a formal notification sent from the employer to the Plan Administrator, typically the insurance company, outlining an employee's qualifying event that may alter their eligibility status for employee benefits. As per the Consolidated Omnibus Budget Reconciliation Act (COBRA) regulations, these notices help ensure proper administration of employee benefits and provide employees with essential information about their rights and options. Types of Qualifying Events: 1. Termination or Reduction in hours: If an employee's employment is terminated or their work hours are significantly reduced, they experience a qualifying event. The MEN serve as notification to the Plan Administrator that the affected employee may be eligible for continued coverage under COBRA. 2. Divorce or Legal Separation: When an employee goes through a divorce or legal separation, their spouse and dependents may lose their eligibility for benefits. Through the MEN, the employer informs the Plan Administrator of the change in the employee's marital status, thereby allowing the Plan Administrator to adjust coverage accordingly. 3. Death of the Employee: In the unfortunate event of an employee's death, the MEN notifies the Plan Administrator to remove the deceased employee from the coverage list. It also helps in ensuring that health insurance benefits are extended to any eligible dependents in accordance with COBRA regulations. 4. Eligibility Age Limitation: Some employee benefit plans have age limitations, such as coverage for dependent children up to a certain age. When a dependent child reaches the age limit, the employer sends an MEN to the Plan Administrator to remove the child from the coverage list, allowing necessary adjustments to be made. 5. Loss of Dependent Status: If an employee's dependent child no longer meets the eligibility criteria defined in the employee benefit plan (e.g., due to marriage, reaching the age limit, or gaining independent coverage), the employer submits an MEN to remove the dependent child from the coverage list. 6. Change in Employment Status: When an employee's employment status shifts, such as moving from part-time to full-time or vice versa, it is important to provide an MEN to the Plan Administrator. This ensures that the employee's benefits align with the new employment arrangement. In Maricopa, Arizona, employers should be familiar with these types of Qualifying Event Notices and understand when and how to submit them to the Plan Administrator. These notices play a vital role in safeguarding employees' rights and maintaining compliance with COBRA regulations. By promptly providing accurate information, employers contribute to the efficient administration of employee benefits during transitional periods.
Maricopa Arizona Qualifying Event Notice Information for Employer to Plan Administrator
Description
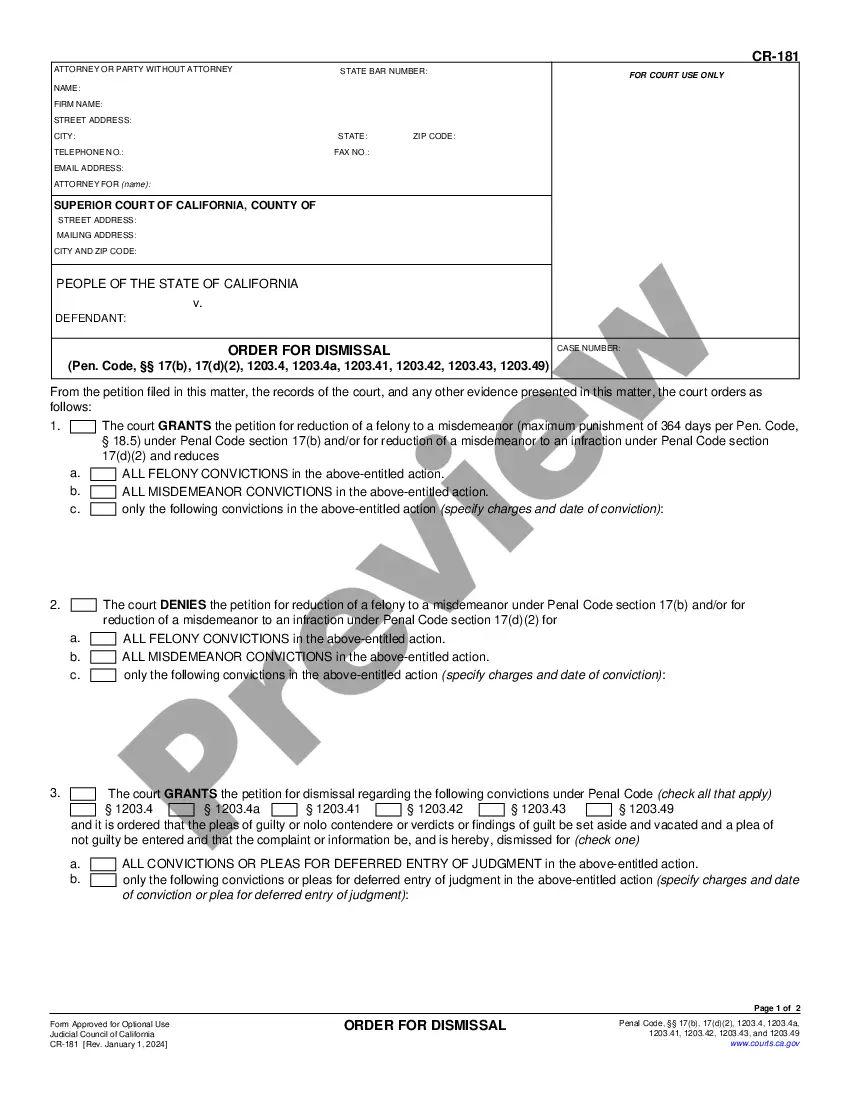
How to fill out Maricopa Arizona Qualifying Event Notice Information For Employer To Plan Administrator?
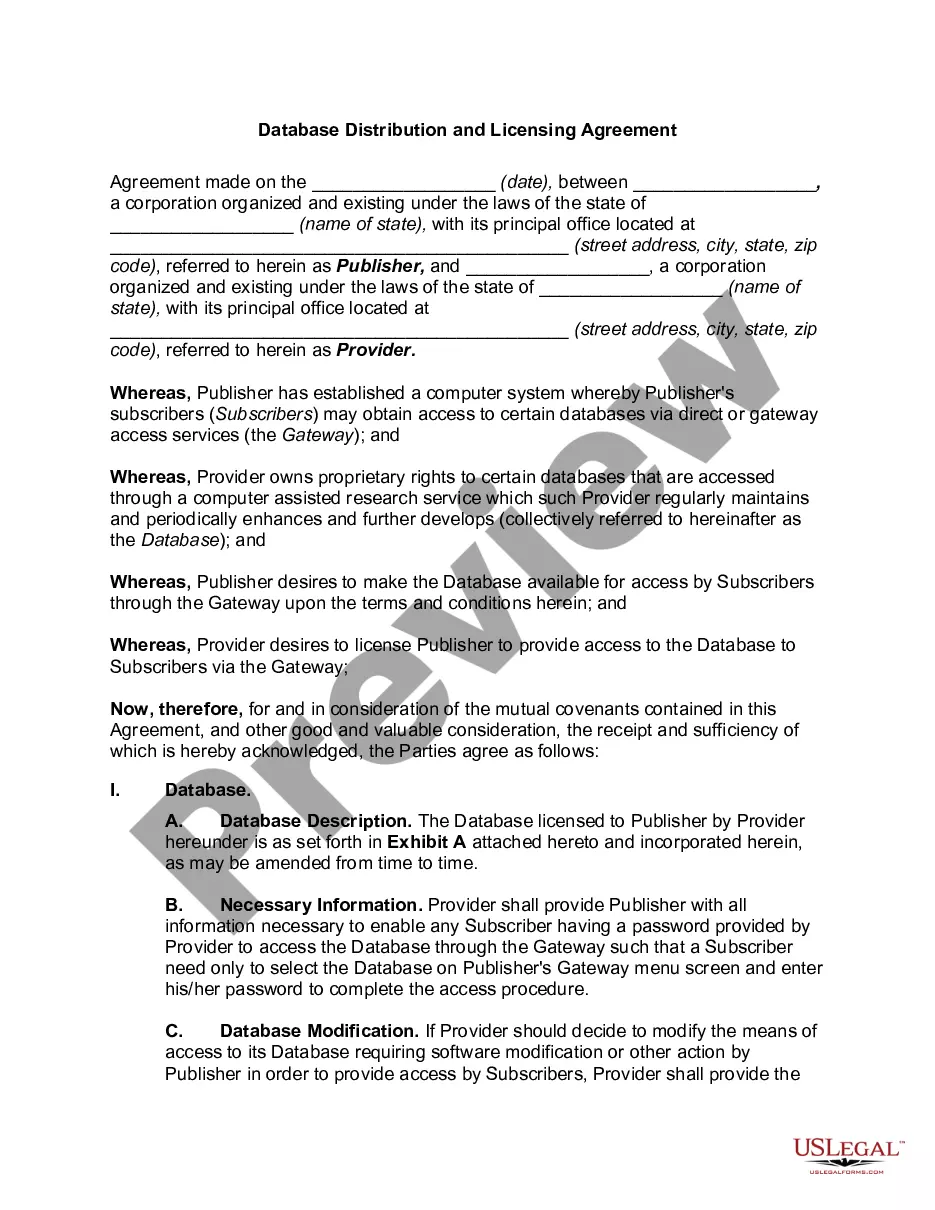
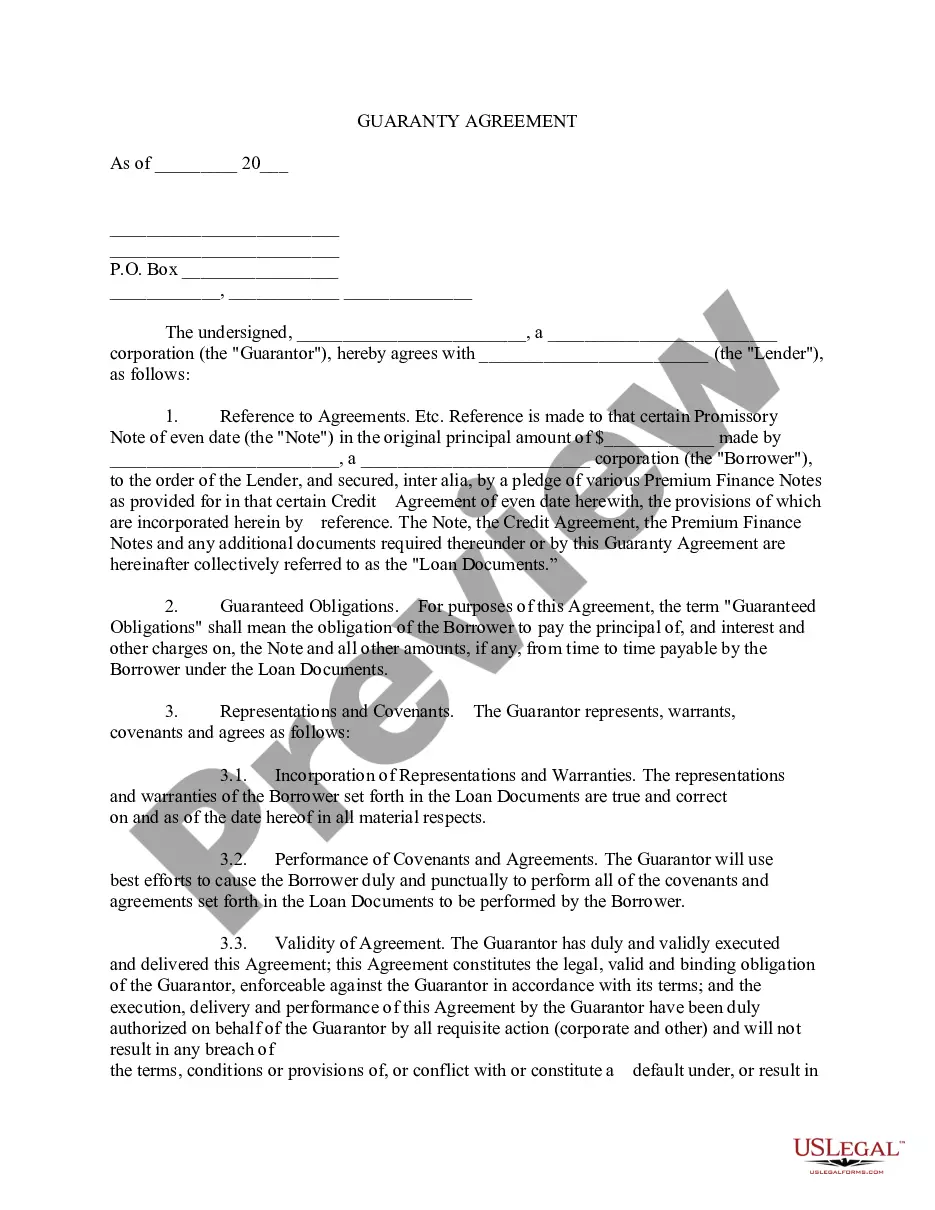
A document routine always goes along with any legal activity you make. Creating a business, applying or accepting a job offer, transferring ownership, and many other life scenarios require you prepare official documentation that varies from state to state. That's why having it all accumulated in one place is so valuable.
US Legal Forms is the largest online collection of up-to-date federal and state-specific legal forms. Here, you can easily find and get a document for any personal or business purpose utilized in your region, including the Maricopa Qualifying Event Notice Information for Employer to Plan Administrator.
Locating samples on the platform is extremely simple. If you already have a subscription to our library, log in to your account, find the sample using the search bar, and click Download to save it on your device. Following that, the Maricopa Qualifying Event Notice Information for Employer to Plan Administrator will be available for further use in the My Forms tab of your profile.
If you are using US Legal Forms for the first time, follow this simple guideline to obtain the Maricopa Qualifying Event Notice Information for Employer to Plan Administrator:
- Make sure you have opened the correct page with your regional form.
- Make use of the Preview mode (if available) and browse through the template.
- Read the description (if any) to ensure the form corresponds to your needs.
- Search for another document via the search tab in case the sample doesn't fit you.
- Click Buy Now when you locate the required template.
- Decide on the appropriate subscription plan, then log in or create an account.
- Select the preferred payment method (with credit card or PayPal) to proceed.
- Choose file format and save the Maricopa Qualifying Event Notice Information for Employer to Plan Administrator on your device.
- Use it as needed: print it or fill it out electronically, sign it, and send where requested.
This is the easiest and most trustworthy way to obtain legal documents. All the templates available in our library are professionally drafted and checked for correspondence to local laws and regulations. Prepare your paperwork and run your legal affairs efficiently with the US Legal Forms!
Form popularity
FAQ
Your group health plan can require you to pay for COBRA continuation coverage. The maximum amount charged to qualified beneficiaries cannot exceed 102 percent of the cost to the plan for similarly situated individuals covered under the plan who have not incurred a qualifying event.
When the qualifying event is the covered employee's termination of employment or reduction in hours of employment, qualified beneficiaries are entitled to 18 months of continuation coverage.
The Consolidated Omnibus Budget Reconciliation Act (COBRA) gives workers and their families who lose their health benefits the right to choose to continue group health benefits provided by their group health plan for limited periods of time under certain circumstances such as voluntary or involuntary job loss,
Gaining a dependent or becoming a dependent through birth or adoption. Getting married. Applicant or dependent lost minimum essential coverage due to termination or change in employment status.
Taking a leave of absence under the Family and Medical Leave Act of 1993 (FMLA) is not a COBRA qualifying event because FMLA requires a covered employer to maintain group health plan benefits for an employee so the employee has no coverage loss.
Your monthly COBRA premiums (or payments) will equal the total cost of the premium under your employer-sponsored health insurance, plus a 2% administration charge. If you've had insurance through your employer for a while, the price to continue that coverage on your own is going to sting.
The Consolidated Omnibus Budget Reconciliation Act (COBRA) gives workers and their families who lose their health benefits the right to choose to continue group health benefits provided by their group health plan for limited periods of time under certain circumstances such as voluntary or involuntary job loss,
Under House bill 1225, the law expands eligibility in the program from businesses with 50 employees to those with 250 or fewer workers. Under the program, the state pays 60 percent of the insurance costs, the employer pays 25 percent and the employee pays the remaining 15 percent.
The following are qualifying events: the death of the covered employee; a covered employee's termination of employment or reduction of the hours of employment; the covered employee becoming entitled to Medicare; divorce or legal separation from the covered employee; or a dependent child ceasing to be a dependent under
You may be able to keep your job-based health plan through COBRA continuation coverage. COBRA is a federal law that may let you pay to stay on your employee health insurance for a limited time after your job ends (usually 18 months). You pay the full premium yourself, plus a small administrative fee.