Mecklenburg North Carolina Qualifying Event Notice Information for Employer to Plan Administrator serves as a crucial communication tool for employers in the county. This descriptive content will outline the primary types of qualifying events in Mecklenburg, as well as provide key information for employers to effectively notify the plan administrator. Keywords: Mecklenburg, North Carolina, Qualifying Event Notice, Information, Employer, Plan Administrator. Types of Mecklenburg North Carolina Qualifying Event Notice Information for Employer to Plan Administrator: 1. Employee Change in Employment Status: This event encompasses various scenarios, such as termination, reduction in hours, leave of absence, retirement, or change in position. Employers must notify the plan administrator within a specific timeframe to ensure the affected employee's benefits properly transition. 2. Marriage or Divorce: When an employee gets married or divorced, they may need to make important adjustments to their benefit plans. Employers should inform the plan administrator immediately upon receiving such news to guarantee an appropriate change in coverage or beneficiary designation. 3. Birth or Adoption of a Child: Welcoming a new member to the family often necessitates the modification of health insurance and other benefits. Employers should promptly inform the plan administrator about births or adoptions to ensure the necessary updates to the employee's coverage are implemented efficiently. 4. Loss of Dependent Status: If an employee's dependent no longer qualifies for coverage, either due to age restrictions or other circumstances, employers need to notify the plan administrator. This event may require a change in benefits or additional documentation. 5. Loss of Other Group Coverage: When an employee or their dependent loses coverage under another employer-sponsored plan, employers must communicate this event to the plan administrator. This information allows for timely enrollment in or adjustments to their existing benefits. 6. COBRA Qualifying Events: COBRA (Consolidated Omnibus Budget Reconciliation Act) qualifying events, such as an employee's termination, reduction in hours, or death, necessitate special attention from employers. These events trigger the need for extended healthcare coverage, and notifying the plan administrator promptly is crucial in ensuring compliance. Information to Include in Mecklenburg North Carolina Qualifying Event Notice for Employer to Plan Administrator: 1. Employee details: Provide the employee's full name, employee ID, contact information, and the qualifying event date. 2. Qualifying event specifics: Clearly state the type of qualifying event that occurred and provide supporting documentation when necessary. 3. Dependent information (if applicable): If the qualifying event involves a dependent, include their full name, date of birth, and any supporting documentation that verifies the change in their status. 4. Coverage adjustment details: Specify the changes required, such as adding, removing, or modifying benefits. Include effective dates and any pertinent information regarding coverage continuation or conversion options. 5. Signature and date: Obtain the employer's signature and date for documentation and record-keeping purposes. By effectively communicating these Mecklenburg North Carolina qualifying events to the plan administrator, employers ensure smooth operations, maintain compliance with applicable regulations, and uphold employee satisfaction through efficient benefit administration.
Mecklenburg North Carolina Qualifying Event Notice Information for Employer to Plan Administrator
Description
How to fill out Mecklenburg North Carolina Qualifying Event Notice Information For Employer To Plan Administrator?
A document routine always goes along with any legal activity you make. Opening a company, applying or accepting a job offer, transferring ownership, and many other life scenarios require you prepare official paperwork that varies from state to state. That's why having it all collected in one place is so beneficial.
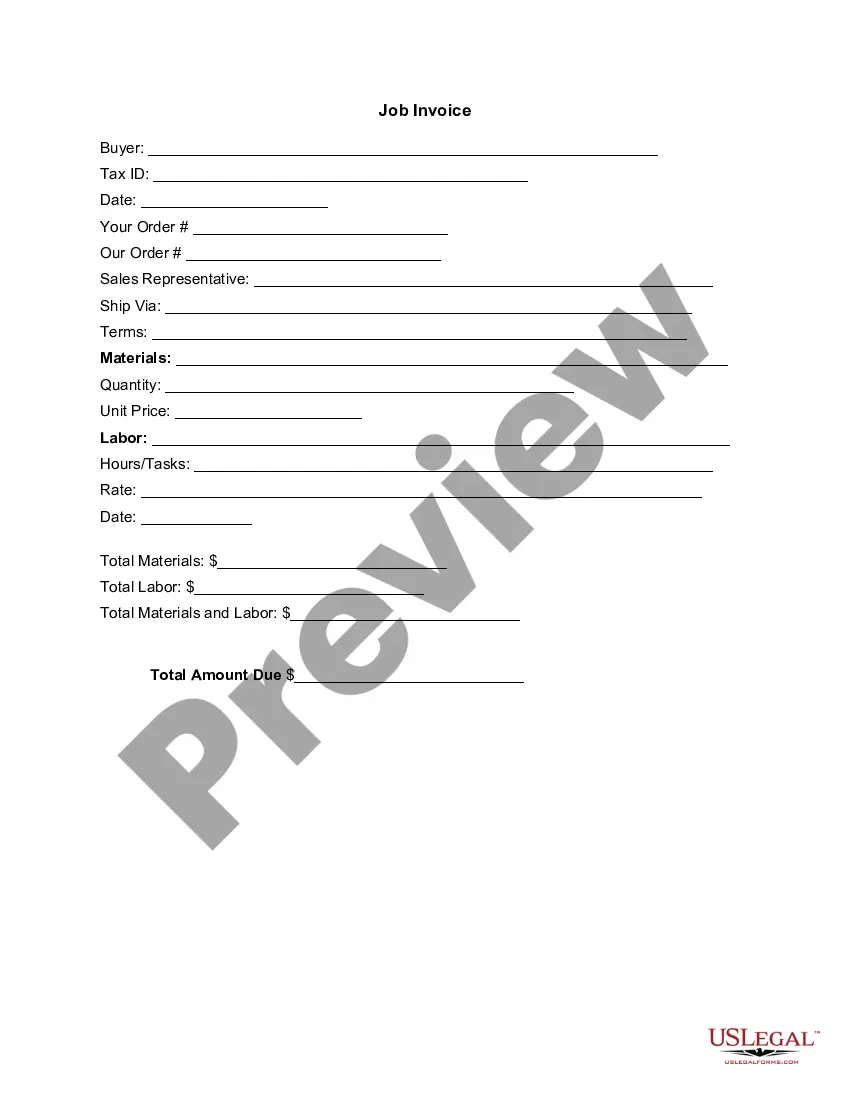
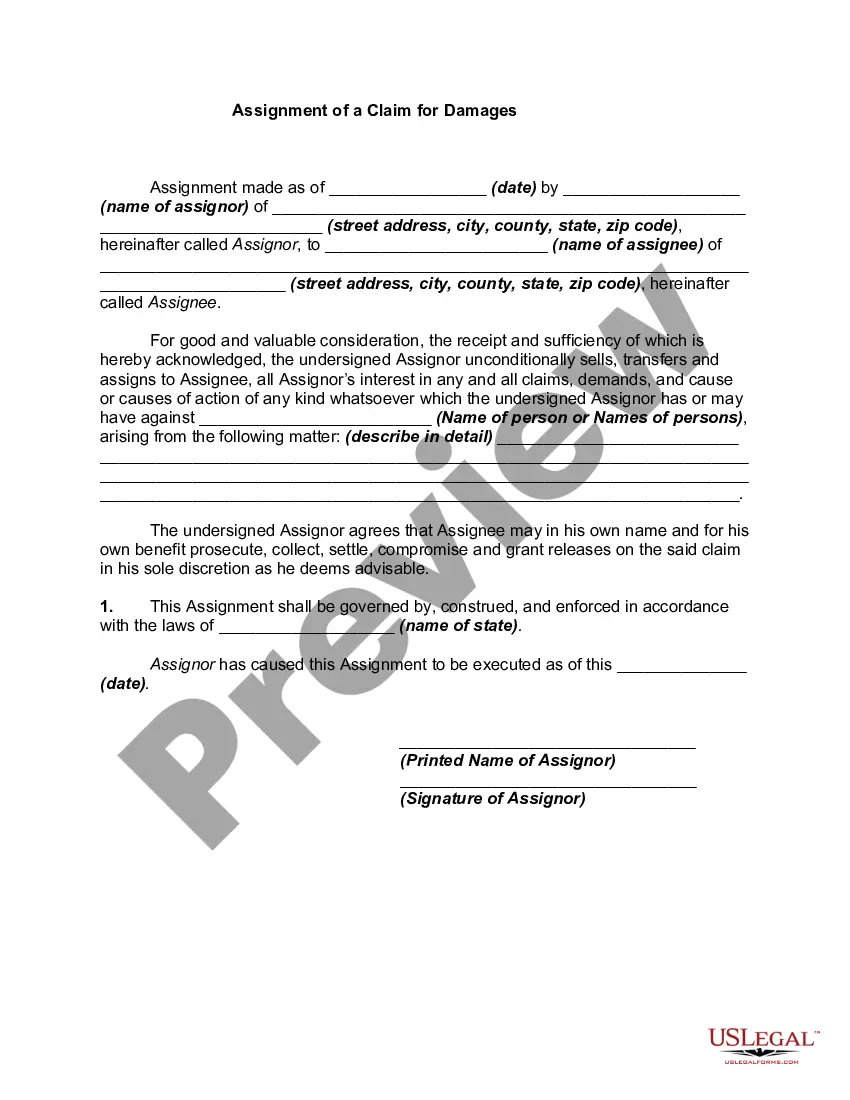
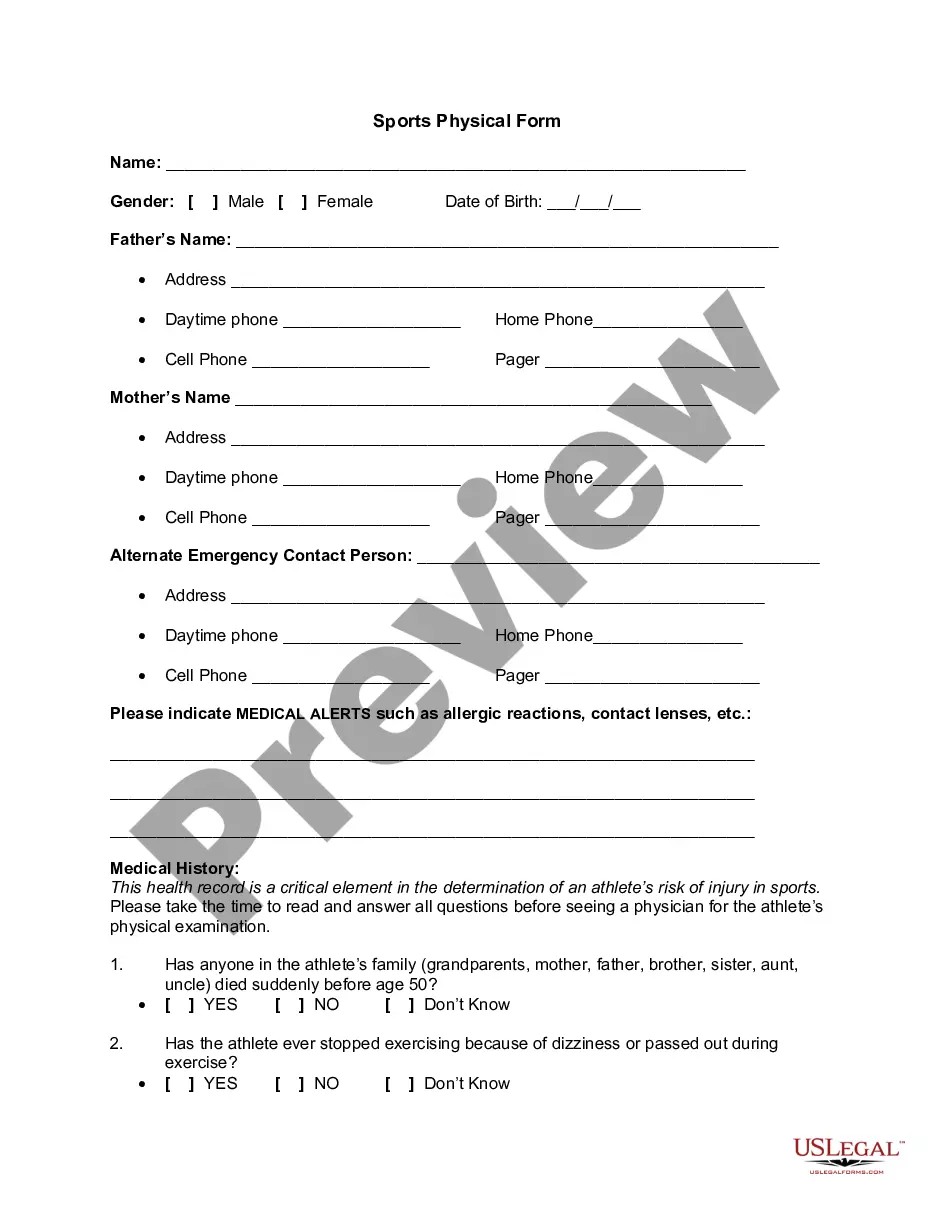
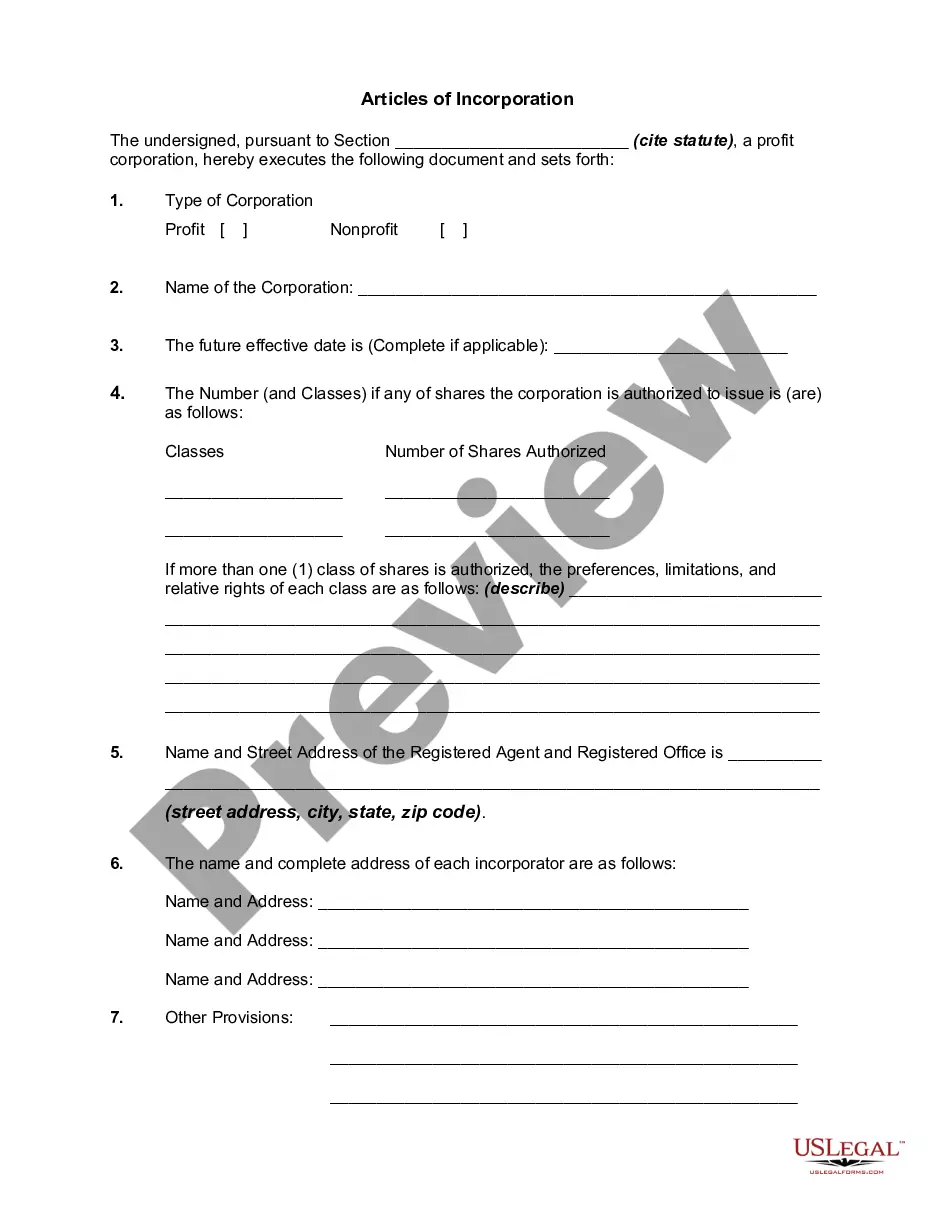
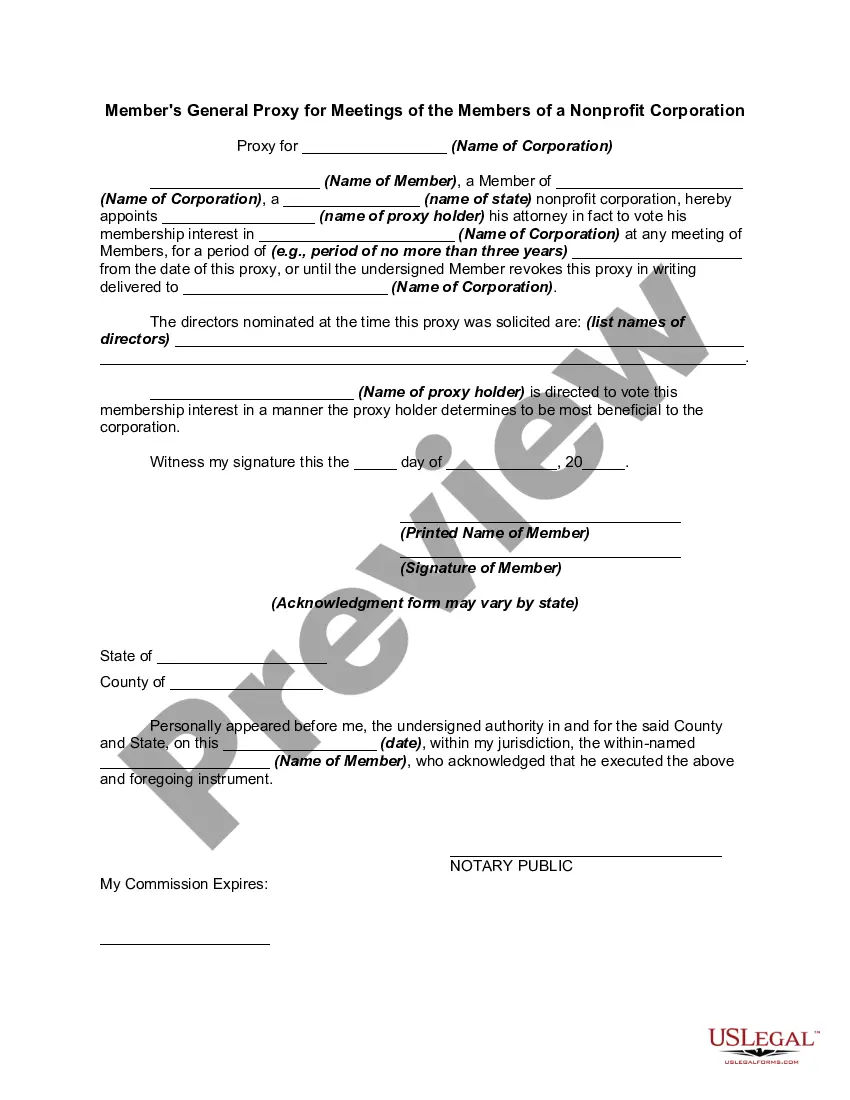
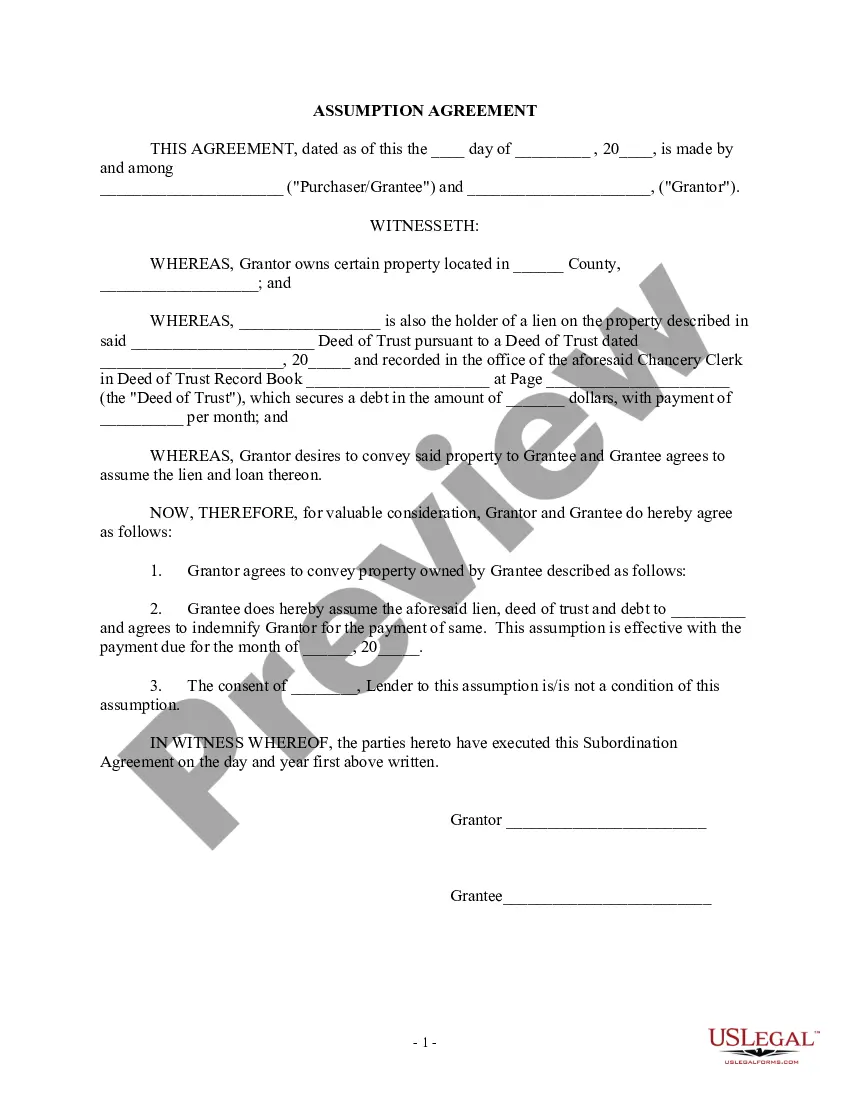
US Legal Forms is the most extensive online library of up-to-date federal and state-specific legal forms. On this platform, you can easily find and get a document for any personal or business purpose utilized in your county, including the Mecklenburg Qualifying Event Notice Information for Employer to Plan Administrator.
Locating samples on the platform is remarkably simple. If you already have a subscription to our service, log in to your account, find the sample using the search bar, and click Download to save it on your device. After that, the Mecklenburg Qualifying Event Notice Information for Employer to Plan Administrator will be accessible for further use in the My Forms tab of your profile.
If you are dealing with US Legal Forms for the first time, follow this quick guideline to obtain the Mecklenburg Qualifying Event Notice Information for Employer to Plan Administrator:
- Make sure you have opened the right page with your local form.
- Use the Preview mode (if available) and scroll through the sample.
- Read the description (if any) to ensure the template corresponds to your needs.
- Look for another document via the search option in case the sample doesn't fit you.
- Click Buy Now when you locate the necessary template.
- Select the appropriate subscription plan, then sign in or register for an account.
- Choose the preferred payment method (with credit card or PayPal) to proceed.
- Opt for file format and download the Mecklenburg Qualifying Event Notice Information for Employer to Plan Administrator on your device.
- Use it as needed: print it or fill it out electronically, sign it, and send where requested.
This is the simplest and most trustworthy way to obtain legal documents. All the samples provided by our library are professionally drafted and verified for correspondence to local laws and regulations. Prepare your paperwork and run your legal affairs efficiently with the US Legal Forms!