Title: Understanding the Phoenix, Arizona Qualifying Event Notice Information for Employers and Plan Administrators Introduction: In Phoenix, Arizona, employers and plan administrators must be well-versed in the Qualifying Event Notice requirements. These notices are essential for ensuring compliance with federal regulations and facilitating proper employee benefits administration. This article provides a detailed description of the Phoenix, Arizona Qualifying Event Notice Information for Employers to Plan Administrators, including key types of qualifying events and their significance. 1. What is a Qualifying Event Notice? A Qualifying Event Notice refers to the notification that an employer or plan administrator must provide to individuals who experience a qualifying event (also known as a life event) that affects their health coverage eligibility, COBRA rights, or other benefits-related matters. 2. Types of Qualifying Events: A. Birth, adoption, or placement for adoption: If an employee or their dependent experiences the birth, adoption, or placement for adoption of a child, they become eligible for a Qualifying Event Notice. B. Marriage or divorce: Whenever an employee gets married or divorced, it triggers a qualifying event, requiring the employer or plan administrator to issue a notice. C. Loss of dependent status: When an employee's dependent no longer qualifies for dependent status under the plan's rules (e.g., due to age), a Qualifying Event Notice becomes necessary. D. Termination or reduction in employment hours: If an employee's employment is terminated or their working hours are reduced, resulting in a loss of health coverage, a Qualifying Event Notice is mandatory. E. Death: Upon the death of an employee, the employer should issue a Qualifying Event Notice to their dependents or beneficiaries, informing them about COBRA continuation or other benefits options. 3. Important Information to Include in a Qualifying Event Notice: A. Explanation of the qualifying event and its impact on benefits eligibility. B. Deadline for individuals to provide required documentation or notify the employer/administrator about the event. C. Guidelines for enrolling in alternative health coverage, such as COBRA. D. The timeframe within which eligible individuals must elect to continue coverage. E. Information on premium costs, payment methods, and due dates for continuation coverage. F. Contact details for the employer or plan administrator to address any questions or concerns regarding the qualifying event or benefits. Conclusion: Phoenix, Arizona's Qualifying Event Notice Information for Employers to Plan Administrators encompasses various types of life events that can affect an individual's benefits eligibility. Employers and plan administrators must familiarize themselves with the different qualifying events and ensure timely and accurate notification is provided. By complying with the Qualifying Event Notice requirements, employers can ensure that employees and their dependents receive the necessary information to make informed decisions regarding their benefits coverage during significant life events.
Phoenix Arizona Qualifying Event Notice Information for Employer to Plan Administrator
Description
How to fill out Phoenix Arizona Qualifying Event Notice Information For Employer To Plan Administrator?
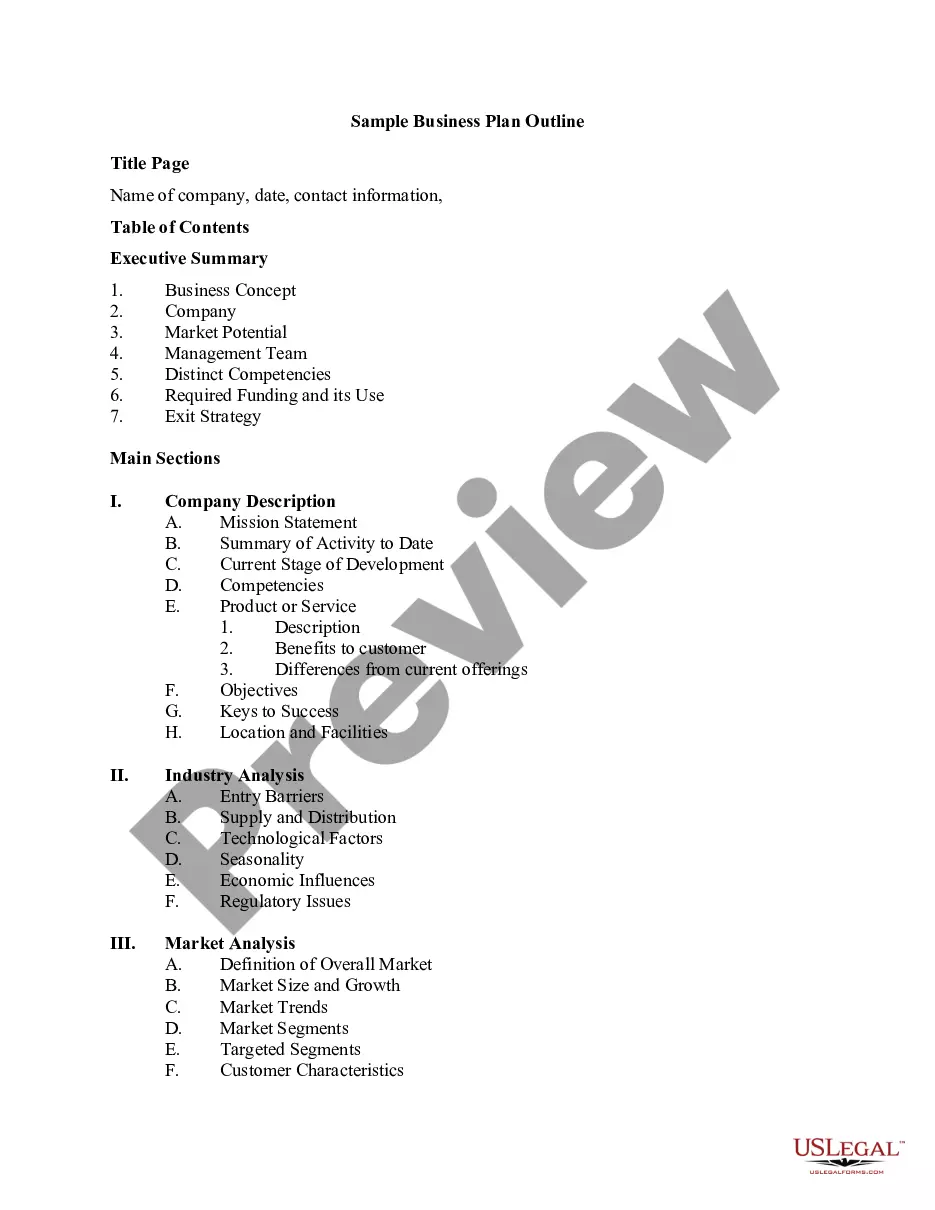
Creating paperwork, like Phoenix Qualifying Event Notice Information for Employer to Plan Administrator, to take care of your legal matters is a challenging and time-consumming task. A lot of situations require an attorney’s participation, which also makes this task not really affordable. However, you can consider your legal affairs into your own hands and deal with them yourself. US Legal Forms is here to save the day. Our website comes with over 85,000 legal forms intended for different scenarios and life circumstances. We ensure each form is compliant with the regulations of each state, so you don’t have to be concerned about potential legal problems associated with compliance.
If you're already familiar with our services and have a subscription with US, you know how effortless it is to get the Phoenix Qualifying Event Notice Information for Employer to Plan Administrator form. Go ahead and log in to your account, download the template, and personalize it to your needs. Have you lost your form? Don’t worry. You can find it in the My Forms folder in your account - on desktop or mobile.
The onboarding process of new users is fairly simple! Here’s what you need to do before getting Phoenix Qualifying Event Notice Information for Employer to Plan Administrator:
- Ensure that your form is compliant with your state/county since the regulations for writing legal paperwork may differ from one state another.
- Discover more information about the form by previewing it or reading a brief description. If the Phoenix Qualifying Event Notice Information for Employer to Plan Administrator isn’t something you were hoping to find, then take advantage of the search bar in the header to find another one.
- Log in or create an account to start utilizing our service and download the form.
- Everything looks good on your end? Hit the Buy now button and choose the subscription plan.
- Pick the payment gateway and enter your payment details.
- Your form is ready to go. You can go ahead and download it.
It’s an easy task to find and buy the needed document with US Legal Forms. Thousands of organizations and individuals are already taking advantage of our rich library. Sign up for it now if you want to check what other perks you can get with US Legal Forms!