Keywords: San Diego California, Qualifying Event Notice, Employer, Plan Administrator, types. Title: Understanding San Diego California's Qualifying Event Notice Information for Employers and Plan Administrators Introduction: In San Diego, California, employers and plan administrators must be well-versed in the detailed information regarding Qualifying Event Notices. These notices are crucial as they inform the necessary parties about significant events that may impact employees' health insurance coverage. This article will provide a comprehensive overview of the various types of San Diego California Qualifying Event Notice Information available for employers and plan administrators to ensure compliance. Types of Qualifying Event Notice Information: 1. Health Insurance Enrollment Changes: When an employee experiences a change in their health insurance enrollment, such as adding a dependent or terminating coverage altogether, a Qualifying Event Notice must be submitted to the plan administrator. This notice ensures that the employee's health coverage is appropriately updated or canceled, allowing for accurate premium calculations and coverage provisions. 2. Employment Status Changes: In the San Diego area, any alteration in an employee's employment status, such as a change in hours, job position, or termination, requires a Qualifying Event Notice to be sent to the plan administrator. This notice enables the necessary adjustments to be made to the employee's health insurance coverage based on their new employment circumstances. 3. Marriage or Divorce: When an employee gets married or divorced, a Qualifying Event Notice must be provided to the plan administrator. This notice guarantees that the employee's health insurance coverage is appropriately updated to include or exclude their spouse or former spouse, based on the legal changes in their marital status. 4. Birth or Adoption of a Child: The birth or adoption of a child is another critical qualifying event that necessitates a notice to the plan administrator. This notice ensures that the employee's health insurance coverage is adjusted to include the newly added dependent(s) and allows for proper premium calculations. 5. Dependent Losing Coverage: If a dependent covered under an employee's health insurance plan becomes ineligible for coverage or loses coverage due to specific circumstances (turning a specified age, no longer being a student, etc.), a Qualifying Event Notice must be submitted. This notice permits the necessary changes to the employee's coverage, such as removing the ineligible dependent from the plan. Conclusion: San Diego, California employers and plan administrators must be well-informed about the various types of Qualifying Event Notice Information to effectively manage employee health insurance coverage. By understanding the importance of timely and accurate notice submissions, employers can maintain compliance and ensure their employees have uninterrupted access to necessary healthcare benefits.
San Diego California Qualifying Event Notice Information for Employer to Plan Administrator
Description
How to fill out San Diego California Qualifying Event Notice Information For Employer To Plan Administrator?
A document routine always accompanies any legal activity you make. Staring a business, applying or accepting a job offer, transferring property, and many other life situations require you prepare official documentation that differs from state to state. That's why having it all collected in one place is so beneficial.
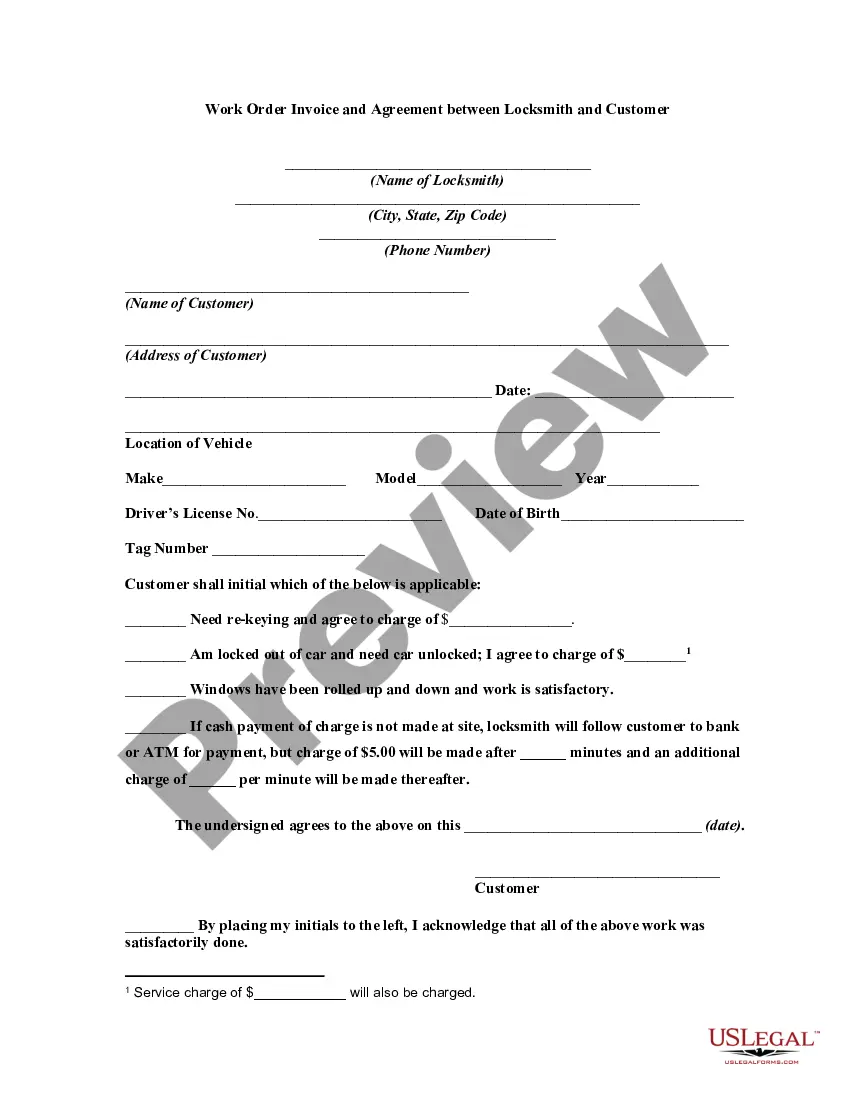
US Legal Forms is the biggest online collection of up-to-date federal and state-specific legal forms. On this platform, you can easily find and download a document for any personal or business objective utilized in your county, including the San Diego Qualifying Event Notice Information for Employer to Plan Administrator.
Locating forms on the platform is extremely simple. If you already have a subscription to our service, log in to your account, find the sample through the search field, and click Download to save it on your device. Following that, the San Diego Qualifying Event Notice Information for Employer to Plan Administrator will be available for further use in the My Forms tab of your profile.
If you are using US Legal Forms for the first time, adhere to this simple guide to obtain the San Diego Qualifying Event Notice Information for Employer to Plan Administrator:
- Ensure you have opened the right page with your regional form.
- Use the Preview mode (if available) and browse through the template.
- Read the description (if any) to ensure the template satisfies your needs.
- Look for another document via the search option in case the sample doesn't fit you.
- Click Buy Now when you find the required template.
- Decide on the suitable subscription plan, then log in or register for an account.
- Select the preferred payment method (with credit card or PayPal) to proceed.
- Choose file format and download the San Diego Qualifying Event Notice Information for Employer to Plan Administrator on your device.
- Use it as needed: print it or fill it out electronically, sign it, and file where requested.
This is the easiest and most trustworthy way to obtain legal documents. All the templates available in our library are professionally drafted and checked for correspondence to local laws and regulations. Prepare your paperwork and run your legal affairs efficiently with the US Legal Forms!
Form popularity
FAQ
In addition, employers can provide COBRA notices electronically (via email, text message, or through a website) during the Outbreak Period, if they reasonably believe that plan participants and beneficiaries have access to these electronic mediums.
You can reach Covered California at (800) 300-1506 or online at . You can apply for individual coverage directly through some health plans off the exchange.
If you need further information about COBRA, ACA, HIPAA, or ERISA, visit the Employee Benefits Security Administration's (EBSA) Website at dol.gov/ebsa/complianceassistance.html. Or you may contact EBSA electronically at askebsa.dol.gov or call toll free 1-866-444-3272.
Administration electronically or call toll free 1-866-444-3272. The Centers for Medicare and Medicaid Services offer information about COBRA provisions for public-sector employees.
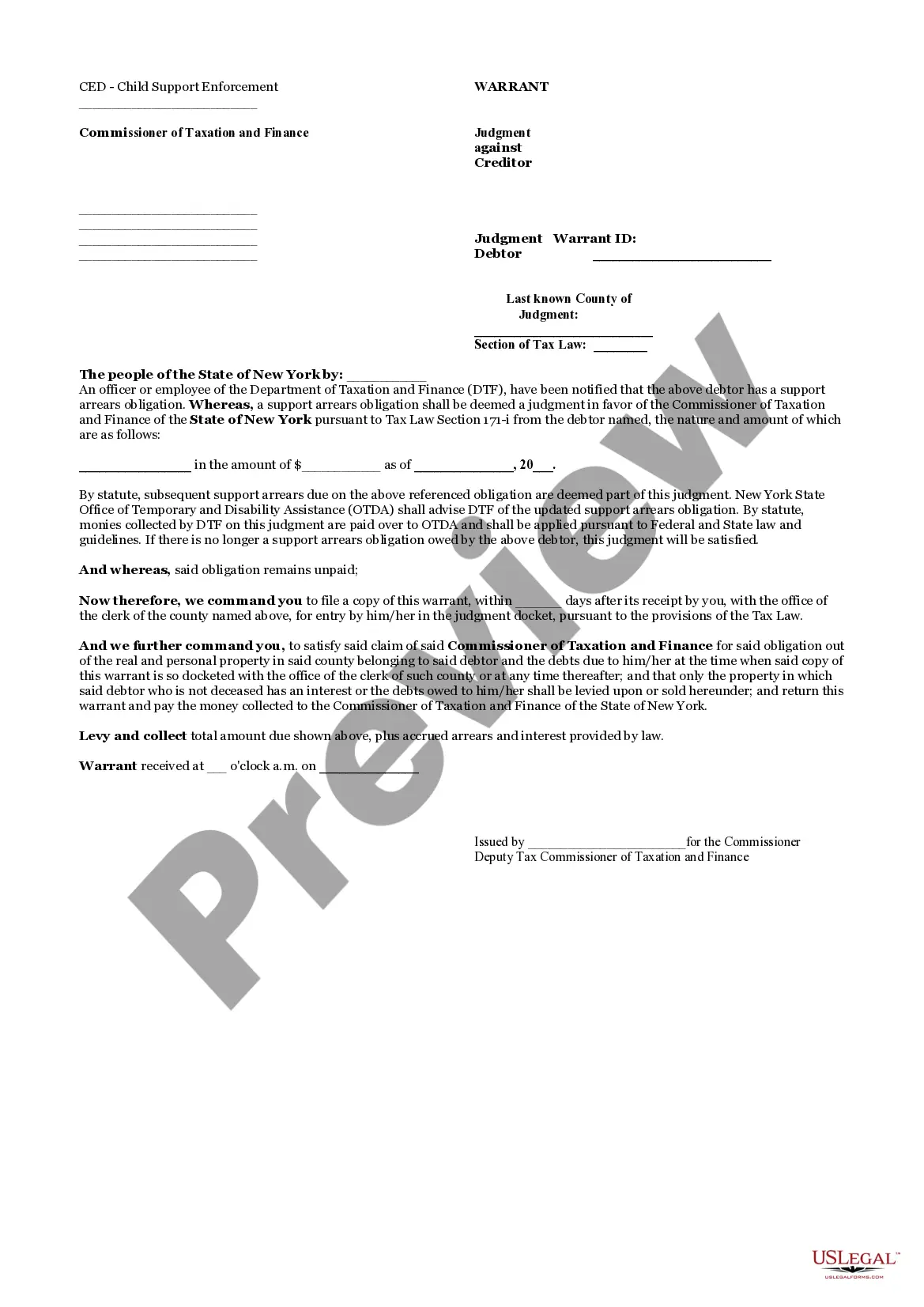
Generally, not all employers sponsoring group health plans must offer COBRA coverage. COBRA generally exempts employers with fewer than 20 full-time employees, as well as certain religious organizations and their affiliates generally exempt from ERISA.
Covered Employers Under federal COBRA, employers with 20 or more employees are usually required to offer COBRA coverage. COBRA applies to plans maintained by private-sector employers (including self-insured plans) and those sponsored by most state and local governments.
The Differences Cal-COBRA applies to employers with 2-19 employees, whereas federal COBRA applies to employers with more than 20 employees. Cal-COBRA offers coverage for up to 36 months, while federal COBRA offers coverage for 18 months for the former employee and up to 36 months for any dependents.
Cal-COBRA is California health coverage protection that requires employers of 2 to 19 employees to provide their employees (and their dependents) the right to continue health insurance benefits when a qualifying event occurs.
Qualifying events include the following: Death of the covered employee. Termination or reduction of hours of the covered employee's employment for reasons other than gross misconduct. Divorce or legal separation from a covered employee.
Under the Employment Retirement Income Security Act of 1974 (ERISA), a penalty of up to $110 per day may be imposed for failing to provide a COBRA notice.