Fairfax Virginia Employer — Plan Administrator Notice to Employee of Unavailability of Continuation: Description: In Fairfax, Virginia, employers are required to provide their employees with specific administrative notices to ensure compliance with various laws and regulations. One such notice is the Fairfax Virginia Employer — Plan Administrator Notice to Employee of Unavailability of Continuation. This notice is essential for informing employees about the unavailability of continuation benefits and their rights in situations where the continuation of benefits cannot be provided. Types of Fairfax Virginia Employer — Plan Administrator Notice to Employee of Unavailability of Continuation: 1. Medical Insurance Continuation Notice: This type of notice is issued when an employee's medical insurance coverage cannot be continued due to circumstances such as the termination of the employer's group health plan, or the employee's ineligibility for federal or state continuation programs like COBRA (Consolidated Omnibus Budget Reconciliation Act). 2. Retirement Benefit Continuation Notice: This notice is distributed to employees when their retirement benefit plans cannot be continued, typically due to the termination or freezing of the employer's retirement plan or the inability to roll over funds to another retirement plan. 3. Disability Benefit Continuation Notice: If a disability benefit plan cannot be continued for an employee, this notice is provided to inform the employee about the termination or unavailability of such benefits. This can occur when the employer's disability plan is discontinued or inaccessible due to legal or operational reasons. Key Keywords: — FairfaVirginiani— - Employer - Plan Administrator — Noticemployedye— - Unavailability of Continuation — AdministrativNoticeic— - Compliance - Medical Insurance — Group HealtPLAla— - COBRA - Retirement Benefit — RetiremenPLAla— - Disability Benefit - Termination Freezingezin— - Ineligibility - Continuation Benefits Note: The specific types of notices may vary based on the employer's benefit plans and the applicable laws in Fairfax, Virginia.
Fairfax Virginia Employer - Plan Administrator Notice to Employee of Unavailability of Continuation
Description
How to fill out Fairfax Virginia Employer - Plan Administrator Notice To Employee Of Unavailability Of Continuation?
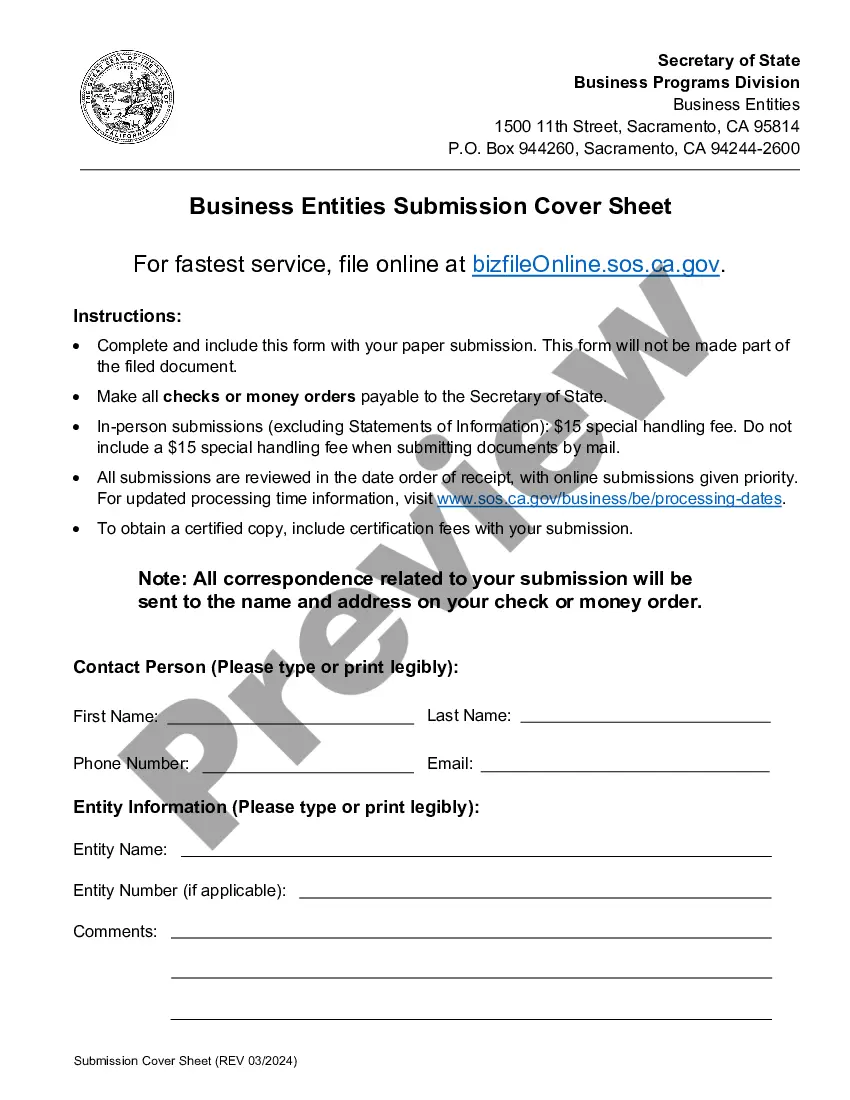
Whether you intend to open your business, enter into a deal, apply for your ID update, or resolve family-related legal issues, you must prepare certain paperwork corresponding to your local laws and regulations. Finding the correct papers may take a lot of time and effort unless you use the US Legal Forms library.
The platform provides users with more than 85,000 professionally drafted and checked legal documents for any personal or business case. All files are grouped by state and area of use, so picking a copy like Fairfax Employer - Plan Administrator Notice to Employee of Unavailability of Continuation is quick and straightforward.
The US Legal Forms library users only need to log in to their account and click the Download key next to the required form. If you are new to the service, it will take you a couple of additional steps to get the Fairfax Employer - Plan Administrator Notice to Employee of Unavailability of Continuation. Adhere to the guidelines below:
- Make sure the sample meets your individual needs and state law regulations.
- Look through the form description and check the Preview if available on the page.
- Use the search tab providing your state above to find another template.
- Click Buy Now to get the file when you find the correct one.
- Select the subscription plan that suits you most to continue.
- Log in to your account and pay the service with a credit card or PayPal.
- Download the Fairfax Employer - Plan Administrator Notice to Employee of Unavailability of Continuation in the file format you require.
- Print the copy or complete it and sign it electronically via an online editor to save time.
Forms provided by our library are multi-usable. Having an active subscription, you can access all of your earlier acquired paperwork at any time in the My Forms tab of your profile. Stop wasting time on a endless search for up-to-date official documentation. Sign up for the US Legal Forms platform and keep your paperwork in order with the most extensive online form collection!
Form popularity
FAQ
Q3: Which employers are required to offer COBRA coverage? COBRA generally applies to all private-sector group health plans maintained by employers that had at least 20 employees on more than 50 percent of its typical business days in the previous calendar year.
Model COBRA notices are provided on the U.S. Department of Labor's COBRA Continuation webpage under the Regulations section. Step 1: Initial Notification.Step 2: Qualifying Event Notices.Step 3: Insurance Carrier Notification.Step 4: Election and Payment.Step 5 (if needed): Late or Missing Payments.
The Consolidated Omnibus Budget Reconciliation Act (COBRA) gives workers and their families who lose their health benefits the right to choose to continue group health benefits provided by their group health plan for limited periods of time under certain circumstances such as voluntary or involuntary job loss,
Virginia regulations require continuation coverage for a period of 12 months from the date of loss of coverage. Virginia regulations require notification to the Qualified Beneficiary of their continuation rights no later than 14 days after knowledge of loss of eligibility.
Cal-COBRA administration requires four basic compliance components: Notifying all eligible group health care participants of their Cal-COBRA rights. Providing timely notice of Cal-COBRA eligibility, enrollment forms, and notice of the duration of coverage and terms of payment after a qualifying event has occurred.
The COBRA election notice should describe all of the necessary information about COBRA premiums, when they are due, and the consequences of payment and nonpayment. Plans cannot require qualified beneficiaries to pay a premium when they make the COBRA election.
A covered employee's spouse who would lose coverage due to a divorce may elect continuation coverage under the plan for a maximum of 36 months. A qualified beneficiary must notify the plan administrator of a qualifying event within 60 days after divorce or legal separation.
COBRA (Consolidated Omnibus Budget Reconciliation Act of 1985) is a federal law that requires employers of 20 or more employees who offer health care benefits to offer the option of continuing this coverage to individuals who would otherwise lose their benefits due to termination of employment, reduction in hours or
Cal-COBRA is a California Law that lets you keep your group health plan when your job ends or your hours are cut. It may also be available to people who have exhausted their Federal COBRA.
Federal COBRA requires continuation coverage be offered to covered employees, their spouses, former spouses, and dependent children. Federal COBRA applies to employers and group health plans that cover 20 or more employees.