Wake, North Carolina is a vibrant city located in the central part of the state. Known for its rich history, scenic beauty, and diverse cultural scene, Wake offers a range of attractions and amenities for residents and visitors alike. One crucial aspect of employment in Wake, North Carolina, is the provision of continuation coverage to employees. Under federal law, employers are required to offer continuation coverage to individuals who experience a qualifying event that would otherwise result in the loss of their health insurance. In some cases, an employer may need to issue a Notice from Employer to Employee Regarding Early Termination of Continuation Coverage. This type of notice informs the employee that their continuation coverage will be terminated ahead of the expected end date. The reasons for early termination may vary but typically include situations where the employee becomes ineligible for continuation coverage due to factors such as finding new employment or failing to make timely premium payments. It is important to note that there might be different types of Wake, North Carolina Notice from Employer to Employee Regarding Early Termination of Continuation Coverage. These could include: 1. Notice for Ineligibility: If an employee becomes ineligible for continuation coverage due to obtaining a new job that provides health insurance or if they fail to make premium payments within the specified time frame, the employer may issue a notice stating the early termination of continuation coverage. 2. Notice of Transition Period: In some cases, the employer may choose to provide a transitional period during which the employee can secure alternative health insurance coverage. This notice would outline the duration of the transition period and any additional information to facilitate the smooth transition and the steps the employee needs to take. 3. Notice of Alternative Coverage Options: If an employer terminates an employee's continuation coverage early, they may be required to provide information about alternative health insurance options available to the employee. This notice would include details such as enrollment periods, eligibility requirements, and contact information for further assistance. In conclusion, while it is necessary for employers in Wake, North Carolina, to offer continuation coverage, circumstances may arise that lead to the early termination of such coverage. Employers must issue appropriate notices to employees, outlining the reasons for termination and providing information about any available alternative coverage options. By doing so, employers ensure compliance with the relevant legal requirements and support their employees in obtaining appropriate healthcare coverage during their transitional period.
Wake North Carolina Notice from Employer to Employee Regarding Early Termination of Continuation Coverage
Description
How to fill out Wake North Carolina Notice From Employer To Employee Regarding Early Termination Of Continuation Coverage?
A document routine always accompanies any legal activity you make. Staring a business, applying or accepting a job offer, transferring property, and many other life scenarios require you prepare official documentation that differs from state to state. That's why having it all accumulated in one place is so valuable.
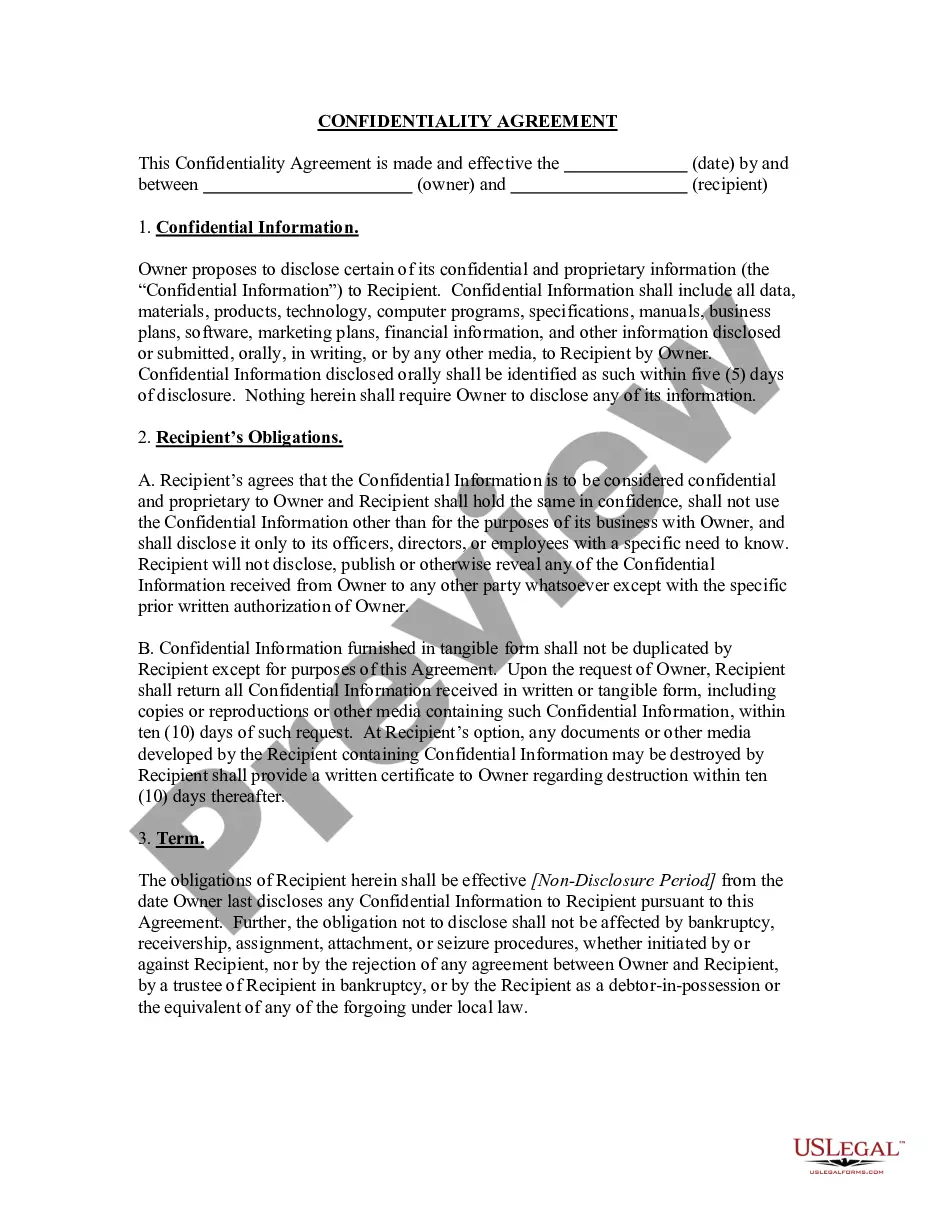
US Legal Forms is the most extensive online collection of up-to-date federal and state-specific legal templates. On this platform, you can easily locate and download a document for any individual or business objective utilized in your county, including the Wake Notice from Employer to Employee Regarding Early Termination of Continuation Coverage.
Locating templates on the platform is extremely simple. If you already have a subscription to our service, log in to your account, find the sample through the search bar, and click Download to save it on your device. Afterward, the Wake Notice from Employer to Employee Regarding Early Termination of Continuation Coverage will be accessible for further use in the My Forms tab of your profile.
If you are using US Legal Forms for the first time, adhere to this quick guideline to obtain the Wake Notice from Employer to Employee Regarding Early Termination of Continuation Coverage:
- Make sure you have opened the correct page with your regional form.
- Make use of the Preview mode (if available) and browse through the template.
- Read the description (if any) to ensure the form satisfies your needs.
- Look for another document using the search option if the sample doesn't fit you.
- Click Buy Now when you find the required template.
- Decide on the suitable subscription plan, then sign in or create an account.
- Select the preferred payment method (with credit card or PayPal) to continue.
- Choose file format and save the Wake Notice from Employer to Employee Regarding Early Termination of Continuation Coverage on your device.
- Use it as needed: print it or fill it out electronically, sign it, and send where requested.
This is the easiest and most reliable way to obtain legal documents. All the templates provided by our library are professionally drafted and checked for correspondence to local laws and regulations. Prepare your paperwork and run your legal affairs efficiently with the US Legal Forms!
Form popularity
FAQ
COBRA generally requires that group health plans sponsored by employers with 20 or more employees in the prior year offer employees and their families the opportunity for a temporary extension of health coverage (called continuation coverage) in certain instances where coverage under the plan would otherwise end.
The COBRA election notice should describe all of the necessary information about COBRA premiums, when they are due, and the consequences of payment and nonpayment. Plans cannot require qualified beneficiaries to pay a premium when they make the COBRA election.
The Department of Labor has developed a model Consolidated Omnibus Budget Reconciliation Act of 1985 (COBRA) continuation coverage extended election notice that the Plan may use to provide the election notice to qualified beneficiaries currently enrolled in COBRA continuation coverage due to reduction in hours or
COBRA (Consolidated Omnibus Budget Reconciliation Act of 1985) is a federal law that requires employers of 20 or more employees who offer health care benefits to offer the option of continuing this coverage to individuals who would otherwise lose their benefits due to termination of employment, reduction in hours or
This notice is intended to provide a summary of your rights, options, and notification responsibilities under COBRA. Should an actual qualifying event occur in the future and coverage is lost, the CalPERS will provide you (and your covered dependents, if any), with the appropriate COBRA election notice at that time.
The Consolidated Omnibus Budget Reconciliation Act of 1986 (COBRA) amended the Public Health Service Act, the Internal Revenue Code and the Employee Retirement Income Security Act (ERISA) to require employers with 20 or more employees to provide temporary continuation of group health coverage in certain situations
The Consolidated Omnibus Budget Reconciliation Act (COBRA) gives workers and their families who lose their health benefits the right to choose to continue group health benefits provided by their group health plan for limited periods of time under certain circumstances such as voluntary or involuntary job loss,
Federal COBRA requires continuation coverage be offered to covered employees, their spouses, former spouses, and dependent children. Federal COBRA applies to employers and group health plans that cover 20 or more employees.
A covered employee's spouse who would lose coverage due to a divorce may elect continuation coverage under the plan for a maximum of 36 months. A qualified beneficiary must notify the plan administrator of a qualifying event within 60 days after divorce or legal separation.
Cal-COBRA is a California Law that lets you keep your group health plan when your job ends or your hours are cut. It may also be available to people who have exhausted their Federal COBRA.