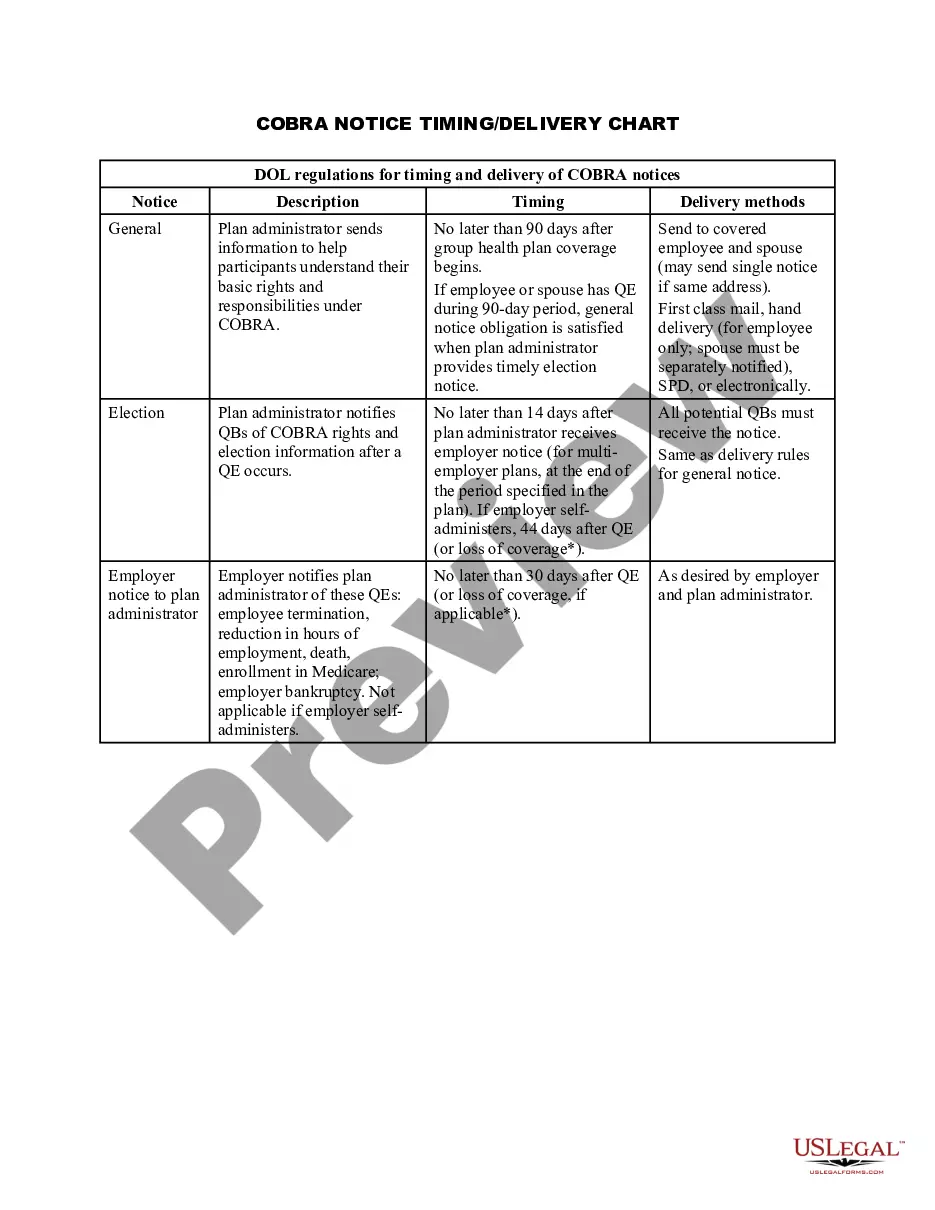
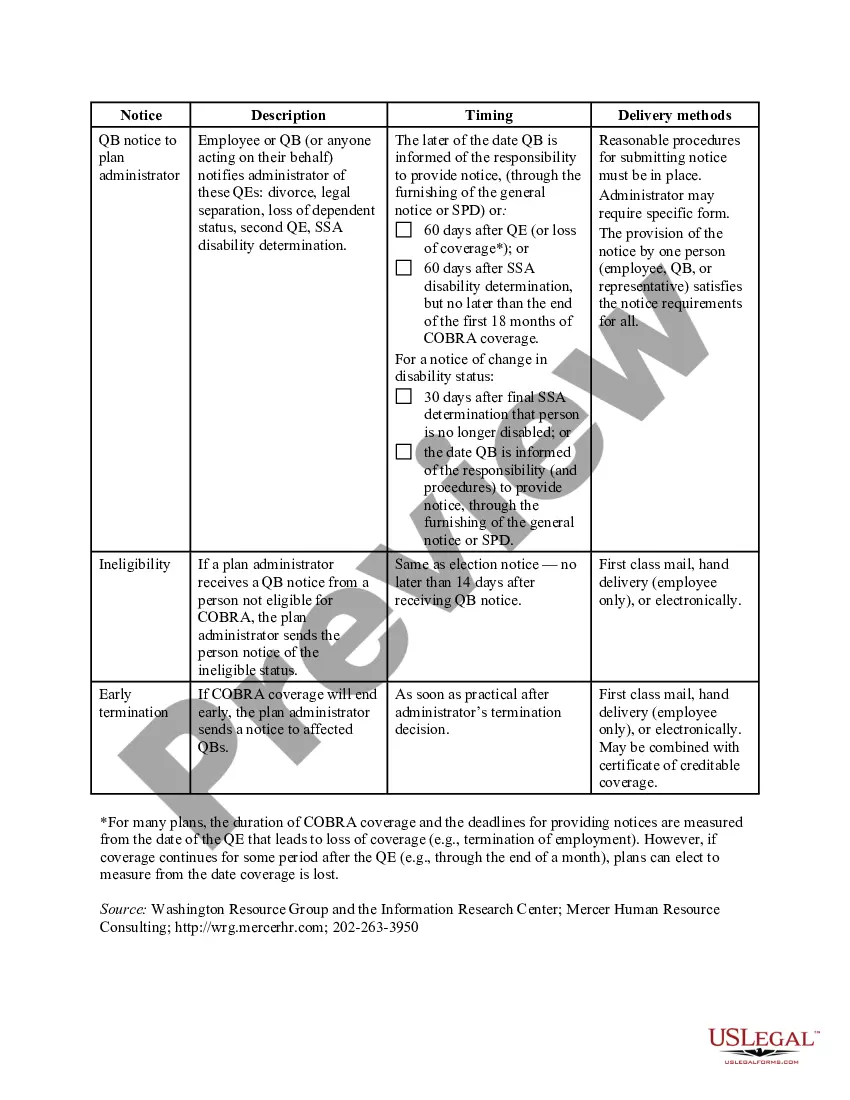
The Bexar Texas COBRA Notice Timing Delivery Chart is a comprehensive document outlining the specific deadlines and requirements for delivering COBRA (Consolidated Omnibus Budget Reconciliation Act) notices in the Bexar County, Texas area. This chart serves as a valuable resource to employers and employees, ensuring compliance with federal regulations regarding healthcare continuation coverage. The Bexar Texas COBRA Notice Timing Delivery Chart outlines the specific notification timelines for various situations such as qualifying events, initial notices, and open enrollment periods. It provides detailed instructions on when the employer must send out the COBRA notices and the timeframes within which employees must respond. Some different types of Bexar Texas COBRA Notice Timing Delivery Charts include: 1. Qualifying Event Chart: This type of chart specifies the specific timing requirements for delivering COBRA notices following a qualifying event such as termination of employment, reduction in work hours, or divorce. It outlines the deadlines for employers to send the initial COBRA notice to individuals and allows them to choose whether they want to continue their healthcare coverage. 2. Open Enrollment Chart: This chart focuses on the periods when employees and dependents can enroll or make changes to their existing COBRA coverage. It outlines the timeframe during which individuals can exercise their right to elect COBRA coverage or make changes to their existing plans. 3. Notice Response Chart: This chart highlights the deadlines for employees to respond to COBRA notices. It specifies the timeframe within which individuals must notify the employer if they want to participate in COBRA coverage or make any changes to their existing plan. By referring to the Bexar Texas COBRA Notice Timing Delivery Chart, both employers and employees can ensure compliance with federal COBRA laws and guarantee the continuation of crucial healthcare coverage during times of transition or change. It serves as a reliable reference tool to avoid potential penalties or the disruption of healthcare benefits for eligible individuals.
Bexar Texas COBRA Notice Timing Delivery Chart
Description
How to fill out Bexar Texas COBRA Notice Timing Delivery Chart?
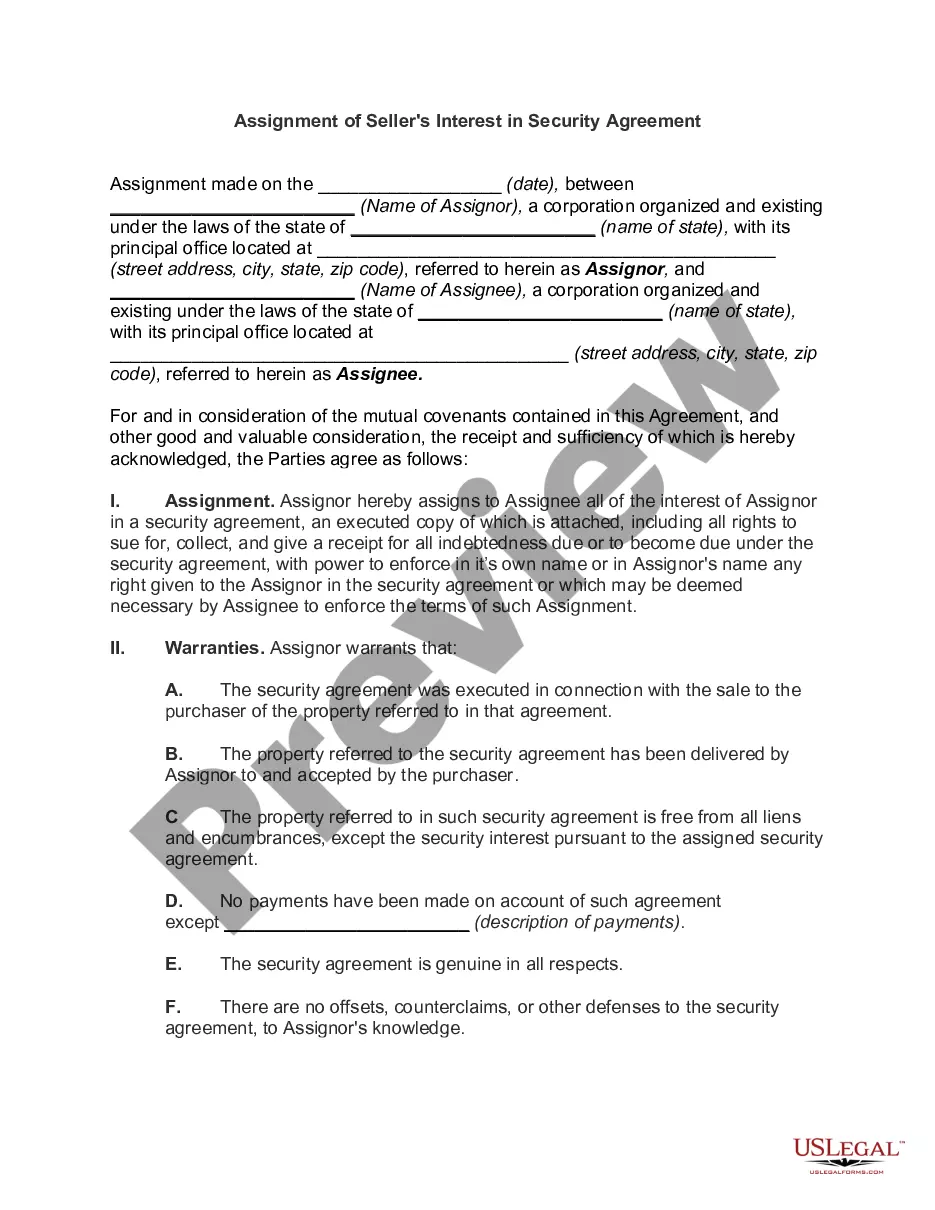
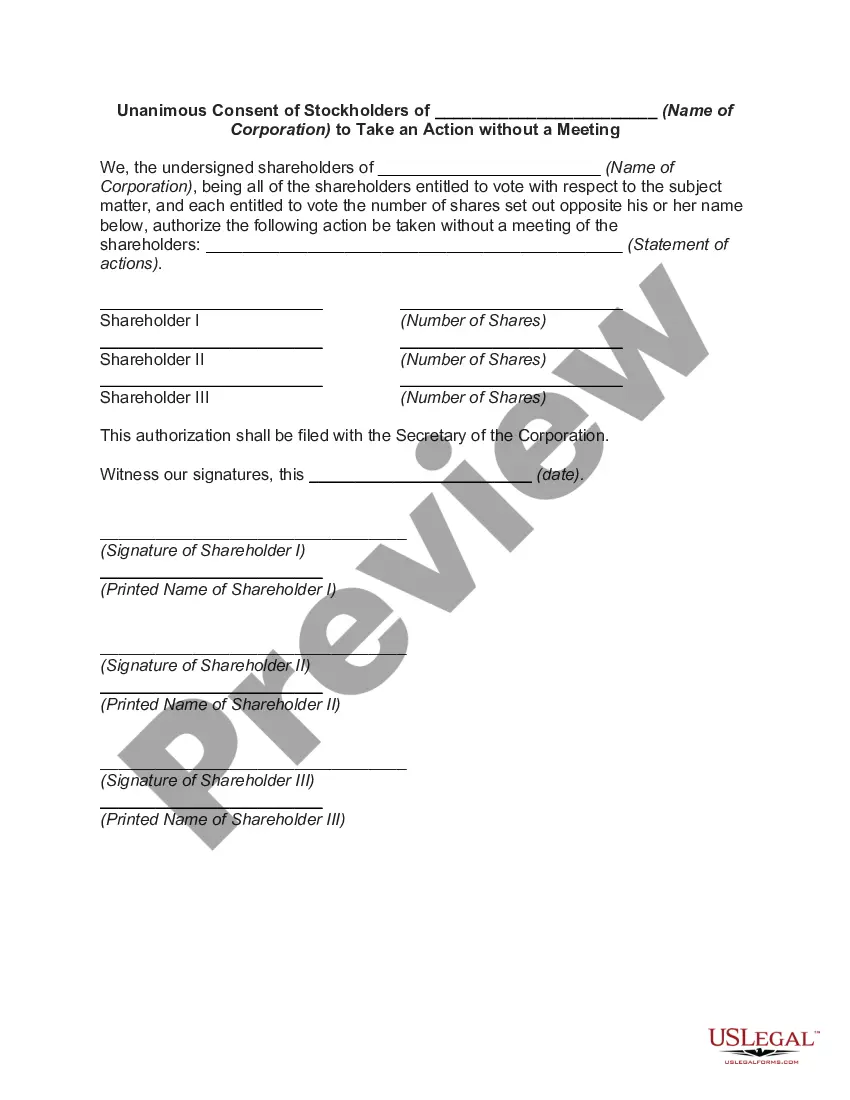
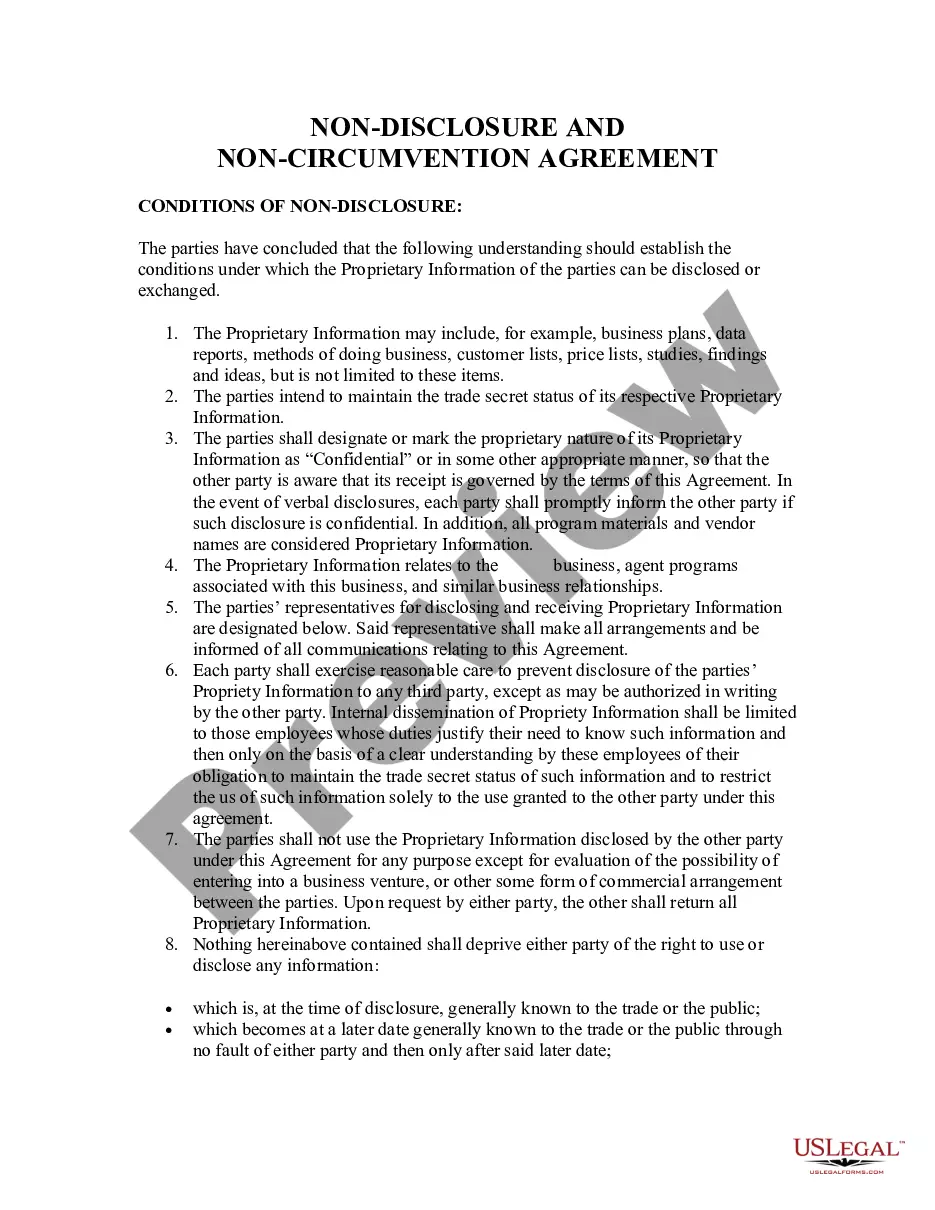
Whether you plan to start your business, enter into a contract, apply for your ID renewal, or resolve family-related legal concerns, you must prepare specific documentation meeting your local laws and regulations. Locating the right papers may take a lot of time and effort unless you use the US Legal Forms library.
The platform provides users with more than 85,000 expertly drafted and verified legal templates for any personal or business case. All files are grouped by state and area of use, so opting for a copy like Bexar COBRA Notice Timing Delivery Chart is quick and easy.
The US Legal Forms website users only need to log in to their account and click the Download button next to the required template. If you are new to the service, it will take you several more steps to obtain the Bexar COBRA Notice Timing Delivery Chart. Adhere to the guide below:
- Make certain the sample fulfills your personal needs and state law requirements.
- Look through the form description and check the Preview if there’s one on the page.
- Utilize the search tab specifying your state above to locate another template.
- Click Buy Now to get the file once you find the correct one.
- Choose the subscription plan that suits you most to proceed.
- Sign in to your account and pay the service with a credit card or PayPal.
- Download the Bexar COBRA Notice Timing Delivery Chart in the file format you need.
- Print the copy or complete it and sign it electronically via an online editor to save time.
Documents provided by our website are reusable. Having an active subscription, you can access all of your earlier purchased paperwork at any moment in the My Forms tab of your profile. Stop wasting time on a endless search for up-to-date official documentation. Sign up for the US Legal Forms platform and keep your paperwork in order with the most extensive online form collection!
Form popularity
FAQ
COBRA Notice of Early Termination of Continuation Coverage Continuation coverage must generally be available for a maximum period (18, 29, or 36 months).
In addition, employers can provide COBRA notices electronically (via email, text message, or through a website) during the Outbreak Period, if they reasonably believe that plan participants and beneficiaries have access to these electronic mediums.
The election notice should include the following information: The name of the plan and the name, address and telephone number of the plan's COBRA administrator. Identification of the qualifying event. Identification of the qualified beneficiaries (by name or by status).
COBRA continuation coverage notices are documents that explain employees' rights under the Consolidated Omnibus Budget Reconciliation Act of 1985. These documents generally contain a variety of information, including the following: The name of the health insurance plan.
A group health plan subject to COBRA is required to provide an initial (or general) COBRA notice to a covered employee or covered spouse only oncewithin 90 days after the individual first becomes covered under the plan. (There is no requirement to provide an initial notice to dependent children.)
You'll have 60 days to enroll in COBRA or another health plan once your benefits end. But keep in mind that delaying enrollment won't save you money. COBRA is always retroactive to the day after your previous coverage ends, and you'll need to pay your premiums for that period too.
There are several other scenarios that may explain why you received a COBRA continuation notice even if you've been in your current position for a long time: You may be enrolled in a new plan annually and, therefore, receive a notice each year. Your employer may have just begun offering a health insurance plan.
Under the Employment Retirement Income Security Act of 1974 (ERISA), a penalty of up to $110 per day may be imposed for failing to provide a COBRA notice.
A group health plan subject to COBRA is required to provide an initial (or general) COBRA notice to a covered employee or covered spouse only oncewithin 90 days after the individual first becomes covered under the plan. (There is no requirement to provide an initial notice to dependent children.)