Fairfax Virginia COBRA Notice Timing Delivery Chart
Description
How to fill out COBRA Notice Timing Delivery Chart?
Drafting documents, such as the Fairfax COBRA Notice Timing Delivery Chart, to manage your legal matters is a challenging and time-consuming endeavor.
Numerous situations necessitate the involvement of a lawyer, which further renders this task somewhat costly.
However, you can take control of your legal matters and manage them independently.
The onboarding process for new clients is equally simple! Here’s what you need to do before downloading the Fairfax COBRA Notice Timing Delivery Chart.
- US Legal Forms is available to assist you.
- Our platform features over 85,000 legal forms crafted for various scenarios and life situations.
- We ensure that each document aligns with the regulations of every state, relieving you of concerns regarding possible legal complications related to compliance.
- If you are already familiar with our services and hold a subscription with US Legal Forms, you understand how simple it is to access the Fairfax COBRA Notice Timing Delivery Chart template.
- Just Log In to your account, download the template, and customize it to fit your requirements.
- Have you misplaced your document? Don’t be concerned.
- You can retrieve it from the My documents section of your account - accessible on both desktop and mobile.
Form popularity
FAQ
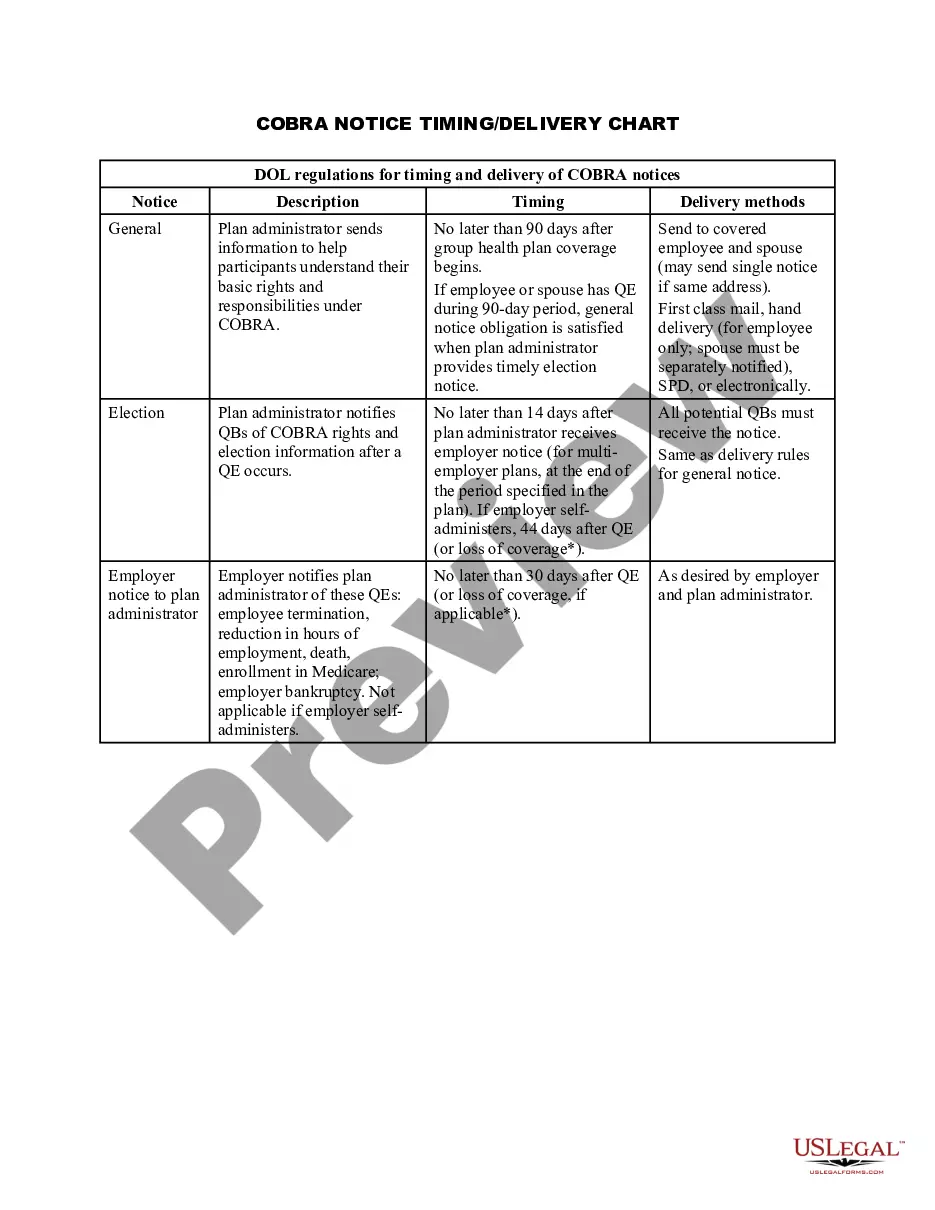
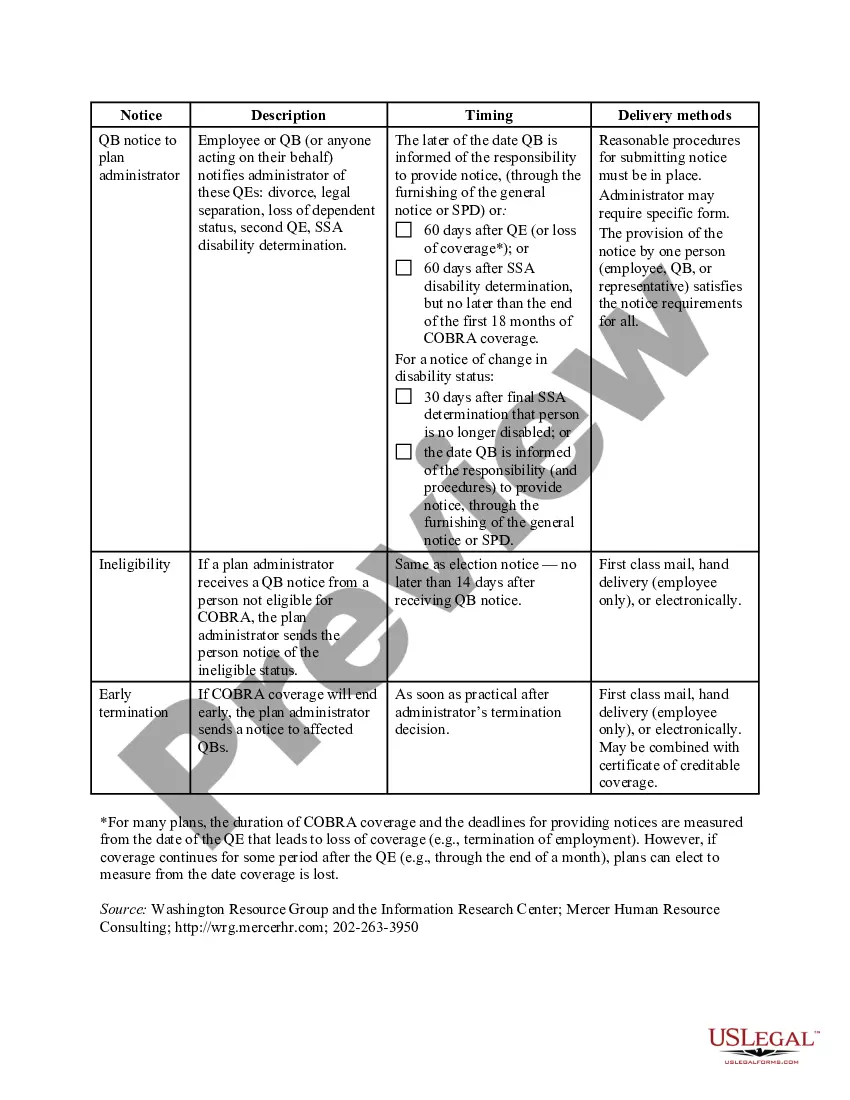
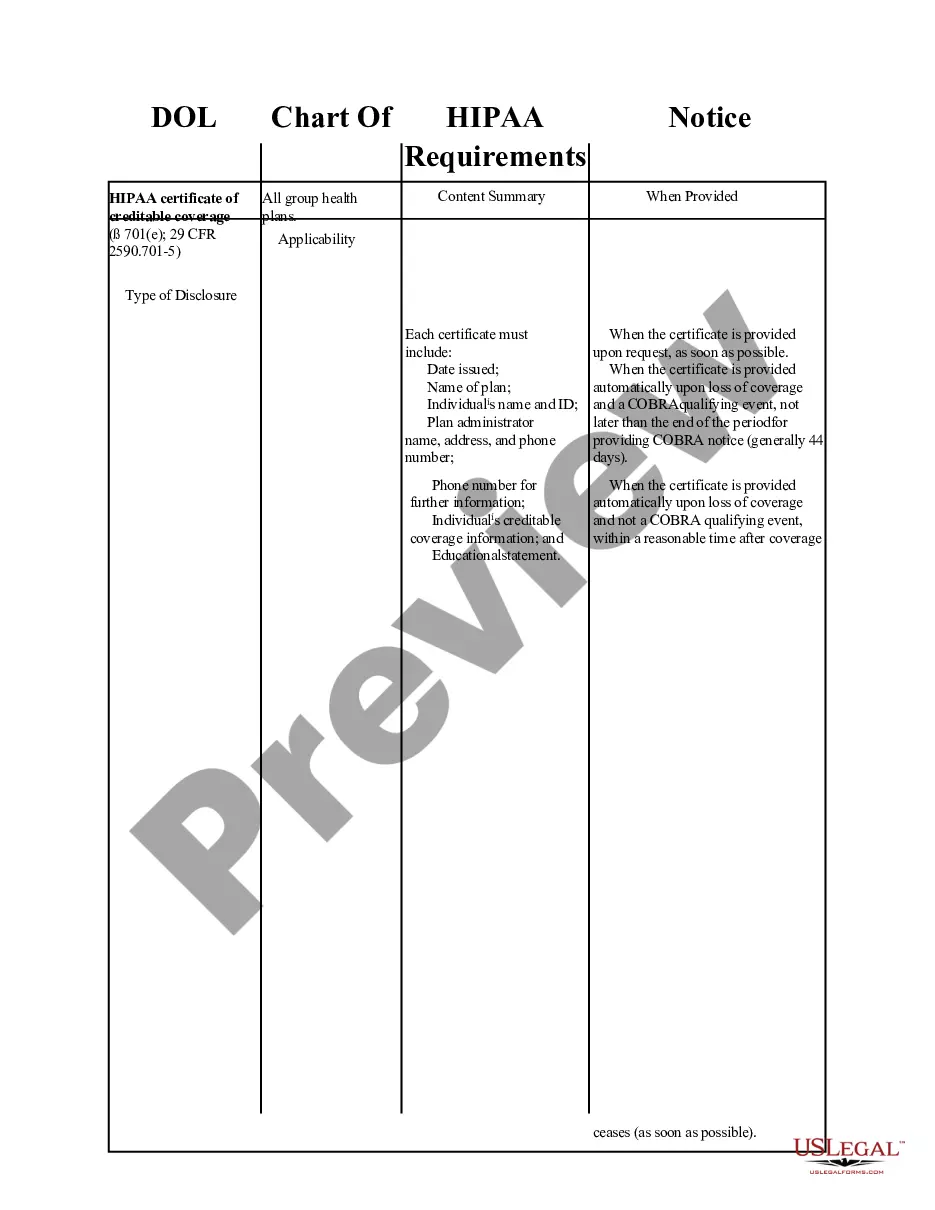
COBRA continuation coverage notices are documents that explain employees' rights under the Consolidated Omnibus Budget Reconciliation Act of 1985. These documents generally contain a variety of information, including the following: The name of the health insurance plan.
The election notice should include the following information: The name of the plan and the name, address and telephone number of the plan's COBRA administrator. Identification of the qualifying event. Identification of the qualified beneficiaries (by name or by status).
The general notice describes general COBRA rights and employee obligations. This notice must be provided to each covered employee and each covered spouse of an employee who becomes covered under the plan. The notice must be provided within the first 90 days of coverage under the group health plan.
Under the Employment Retirement Income Security Act of 1974 (ERISA), a penalty of up to $110 per day may be imposed for failing to provide a COBRA notice.
Your employer must mail you the COBRA information and forms within 14 days after receiving notification of the qualifying event. You are responsible for making sure your COBRA coverage goes into and stays in effect - if you do not ask for COBRA coverage before the deadline, you may lose your right to COBRA coverage.
The COBRA election notice should describe all of the necessary information about COBRA premiums, when they are due, and the consequences of payment and nonpayment. Plans cannot require qualified beneficiaries to pay a premium when they make the COBRA election.
The Department of Labor has developed a model Consolidated Omnibus Budget Reconciliation Act of 1985 (COBRA) continuation coverage extended election notice that the Plan may use to provide the election notice to qualified beneficiaries currently enrolled in COBRA continuation coverage due to reduction in hours or
In addition, employers can provide COBRA notices electronically (via email, text message, or through a website) during the Outbreak Period, if they reasonably believe that plan participants and beneficiaries have access to these electronic mediums.