Houston, Texas General Notice of Preexisting Condition Exclusion is an important document that outlines the exclusion of coverage for preexisting medical conditions. This notice is typically associated with health insurance plans or policies offered in Houston, Texas. A preexisting condition refers to any illness, injury, or medical condition that the individual seeking coverage had before the commencement of the insurance policy. The purpose of the Houston, Texas General Notice of Preexisting Condition Exclusion is to inform policyholders about the limitations placed on coverage for these preexisting conditions. By understanding the details of this notice, individuals can better comprehend their health insurance coverage and make informed decisions when seeking medical treatment. It is crucial to review this notice thoroughly to understand what types of medical conditions may be excluded from coverage. While the specific content may vary between insurance providers, the Houston, Texas General Notice of Preexisting Condition Exclusion typically includes information such as: 1. Definition of preexisting condition: This section explains what qualifies as a preexisting condition under the insurance policy. It may outline the timeframe within which a condition must have been present to be considered preexisting. 2. Exclusion period: The notice clarifies the duration for which preexisting conditions will not be covered. This exclusion period can range from a few months to a year, depending on the insurance policy. 3. Exceptions: Some policies may mention exceptions to the exclusion where certain preexisting conditions may be covered even within the specified exclusion period. These exceptions are typically stated in the notice. 4. Notification requirements: The notice may outline any obligations the policyholder has to inform the insurance company about their preexisting conditions. Some policies may require the policyholder to disclose any known preexisting conditions during the application process. 5. Appeal process: If a claim related to a preexisting condition is denied or contested, the notice might briefly explain the process by which a policyholder can appeal the decision. It is crucial to be aware that the Houston, Texas General Notice of Preexisting Condition Exclusion may differ between insurance providers and policy types. Specific types of such notices include Group Health Insurance Notices, Individual Health Insurance Notices, Medicare Advantage Plan Notices, and Health Maintenance Organization (HMO) Notices. Understanding the Houston, Texas General Notice of Preexisting Condition Exclusion is essential for individuals seeking health insurance coverage in Houston, Texas. It provides transparency regarding coverage limitations for preexisting conditions, enabling policyholders to plan and manage their medical expenses effectively. By carefully reviewing this notice, individuals can make informed choices that best suit their healthcare needs.
Houston Texas General Notice of Preexisting Condition Exclusion
Description
How to fill out Houston Texas General Notice Of Preexisting Condition Exclusion?
A document routine always goes along with any legal activity you make. Opening a business, applying or accepting a job offer, transferring ownership, and many other life scenarios require you prepare formal documentation that varies from state to state. That's why having it all collected in one place is so beneficial.
US Legal Forms is the largest online library of up-to-date federal and state-specific legal forms. Here, you can easily find and download a document for any individual or business objective utilized in your region, including the Houston General Notice of Preexisting Condition Exclusion.
Locating templates on the platform is remarkably straightforward. If you already have a subscription to our service, log in to your account, find the sample through the search field, and click Download to save it on your device. Following that, the Houston General Notice of Preexisting Condition Exclusion will be available for further use in the My Forms tab of your profile.
If you are using US Legal Forms for the first time, follow this quick guideline to obtain the Houston General Notice of Preexisting Condition Exclusion:
- Ensure you have opened the correct page with your regional form.
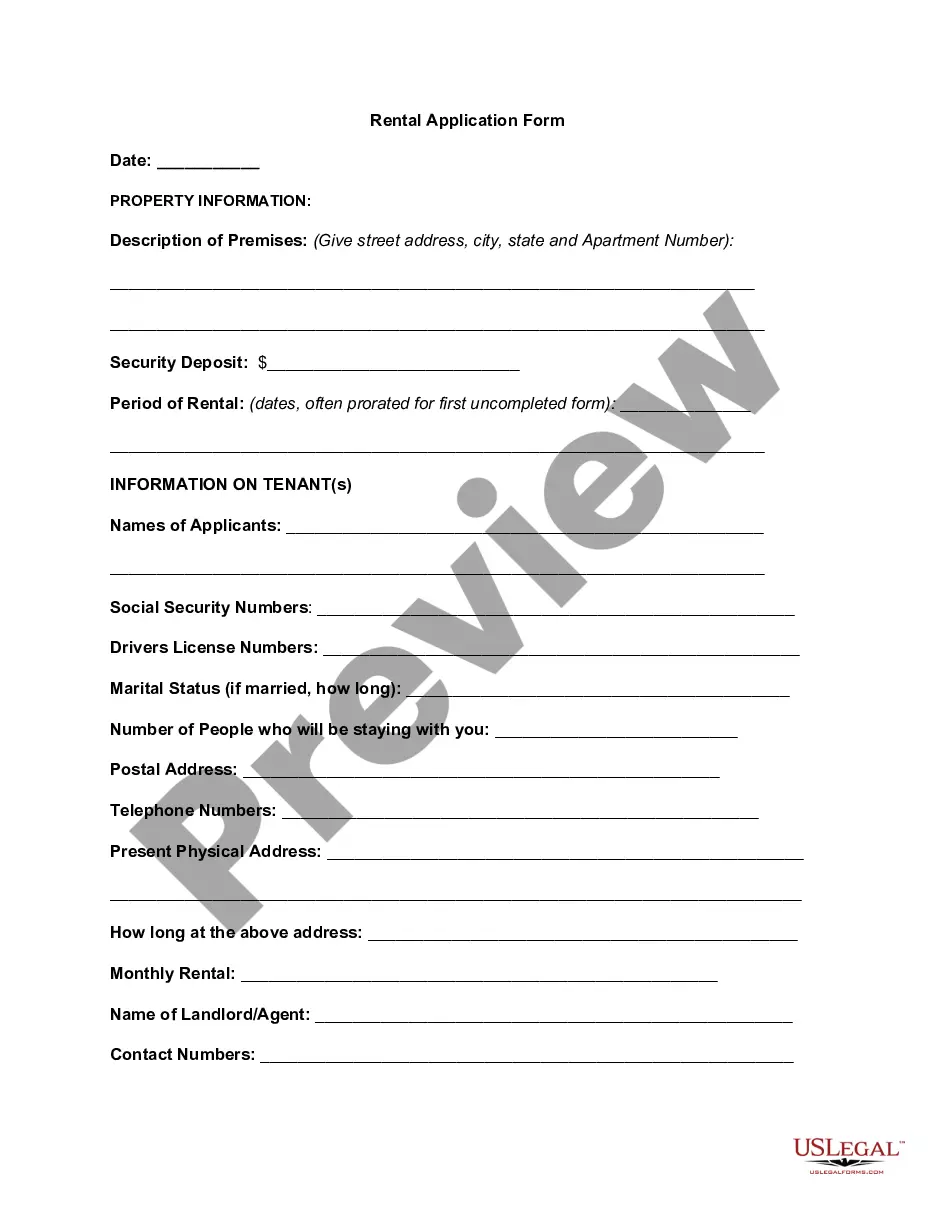
- Use the Preview mode (if available) and scroll through the sample.
- Read the description (if any) to ensure the form corresponds to your requirements.
- Search for another document using the search option if the sample doesn't fit you.
- Click Buy Now once you locate the necessary template.
- Select the appropriate subscription plan, then log in or register for an account.
- Choose the preferred payment method (with credit card or PayPal) to continue.
- Opt for file format and save the Houston General Notice of Preexisting Condition Exclusion on your device.
- Use it as needed: print it or fill it out electronically, sign it, and file where requested.
This is the simplest and most trustworthy way to obtain legal paperwork. All the templates provided by our library are professionally drafted and checked for correspondence to local laws and regulations. Prepare your paperwork and manage your legal affairs effectively with the US Legal Forms!