Riverside California General Notice of Preexisting Condition Exclusion
Description
How to fill out Riverside California General Notice Of Preexisting Condition Exclusion?
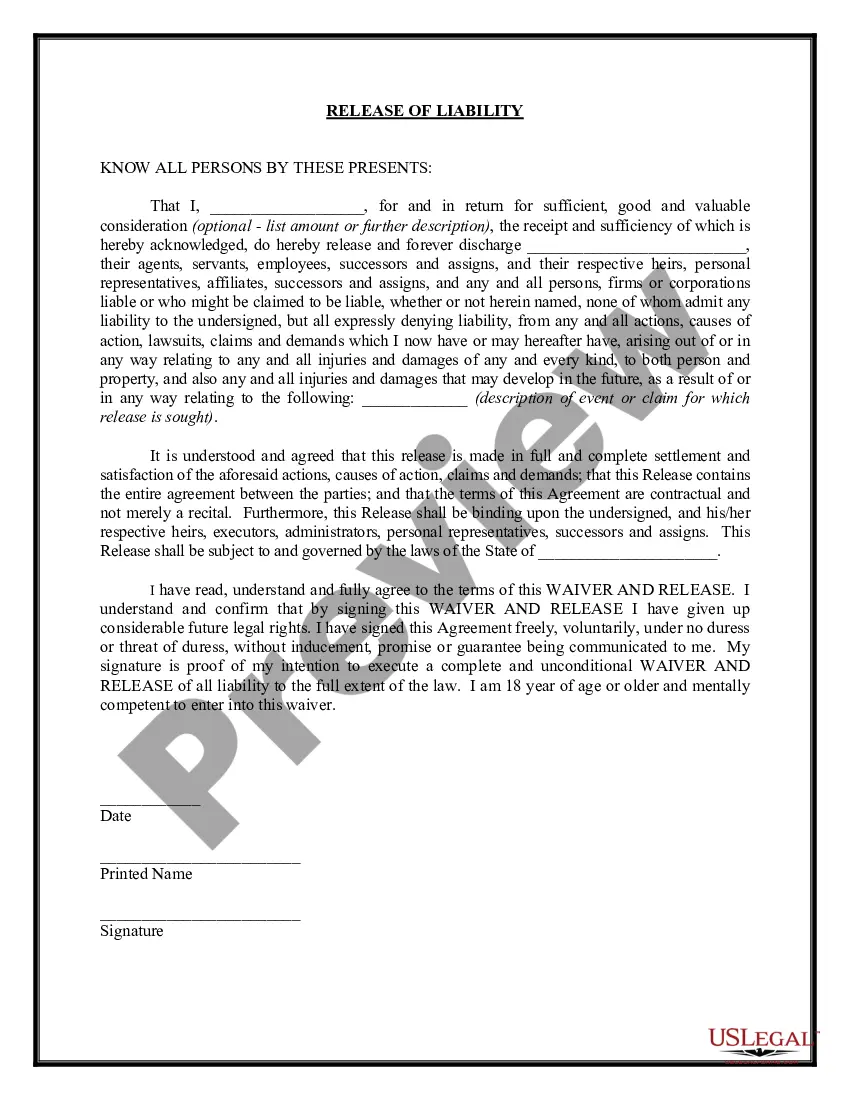
Are you looking to quickly draft a legally-binding Riverside General Notice of Preexisting Condition Exclusion or probably any other document to handle your personal or corporate affairs? You can go with two options: hire a legal advisor to write a legal document for you or draft it completely on your own. The good news is, there's an alternative option - US Legal Forms. It will help you receive professionally written legal paperwork without paying sky-high fees for legal services.
US Legal Forms offers a rich collection of over 85,000 state-specific document templates, including Riverside General Notice of Preexisting Condition Exclusion and form packages. We offer documents for a myriad of life circumstances: from divorce paperwork to real estate documents. We've been out there for more than 25 years and got a spotless reputation among our clients. Here's how you can become one of them and obtain the necessary document without extra troubles.
- First and foremost, double-check if the Riverside General Notice of Preexisting Condition Exclusion is tailored to your state's or county's regulations.
- In case the document includes a desciption, make sure to verify what it's suitable for.
- Start the searching process over if the form isn’t what you were hoping to find by utilizing the search box in the header.
- Choose the plan that best fits your needs and move forward to the payment.
- Choose the file format you would like to get your document in and download it.
- Print it out, fill it out, and sign on the dotted line.
If you've already registered an account, you can easily log in to it, locate the Riverside General Notice of Preexisting Condition Exclusion template, and download it. To re-download the form, just head to the My Forms tab.
It's stressless to buy and download legal forms if you use our catalog. In addition, the templates we provide are reviewed by law professionals, which gives you greater peace of mind when writing legal affairs. Try US Legal Forms now and see for yourself!
Form popularity
FAQ
Yes. Under the Affordable Care Act, health insurance companies can't refuse to cover you or charge you more just because you have a pre-existing condition that is, a health problem you had before the date that new health coverage starts. They also can't charge women more than men.
Clinical Nurse Specialist, Kay Greveson, explains: A pre-existing medical condition can be affected by changes in temperature and climate and should always be declared, even if it is being controlled by medication.
A medical illness or injury that you have before you start a new health care plan may be considered a pre-existing condition. Conditions like diabetes, COPD, cancer, and sleep apnea, may be examples of pre-existing health conditions. They tend to be chronic or long-term.
The time period during which a health plan won't pay for care relating to a pre-existing condition. Under a job-based plan, this cannot exceed 12 months for a regular enrollee or 18 months for a late-enrollee.
The time period during which a health plan won't pay for care relating to a pre-existing condition. Under a job-based plan, this cannot exceed 12 months for a regular enrollee or 18 months for a late-enrollee.
However, a feature of a travel insurance policy known as a pre-existing medical condition exclusion waiver could let you, for instance, cancel a trip due to a flare up of an existing condition and then be reimbursed for nonrefundable travel costs.
In California, group health plans can limit or exclude coverage for pre-existing conditions for adults (age 19 and older) for up to six months from the date coverage begins.
Conditions for Exclusion HIPAA did allow insurers to refuse to cover pre-existing medical conditions for up to the first 12 months after enrollment, or 18 months in the case of late enrollment.
Health insurance companies cannot refuse coverage or charge you more just because you have a pre-existing condition that is, a health problem you had before the date that new health coverage starts.
Health insurers can no longer charge more or deny coverage to you or your child because of a pre-existing health condition like asthma, diabetes, or cancer, as well as pregnancy. They cannot limit benefits for that condition either.