Salt Lake Utah General Notice of Preexisting Condition Exclusion: Explained The Salt Lake Utah General Notice of Preexisting Condition Exclusion is a crucial aspect of health insurance policies. It refers to the provision that allows insurance companies to exclude coverage for preexisting medical conditions for a specified period of time. This exclusion is important for insurance providers to manage costs and mitigate the risk of individuals seeking coverage solely for existing health issues. A preexisting condition is any injury, illness, or medical condition that existed before the start date of a health insurance policy. Examples of preexisting conditions may include chronic illnesses like diabetes, heart disease, cancer, asthma, or any condition for which medical advice, diagnosis, care or treatment was received or recommended within a specific period. The Salt Lake Utah General Notice of Preexisting Condition Exclusion ensures that individuals who have preexisting conditions are made aware of the restrictions surrounding their coverage. It promotes transparency and allows policyholders to make informed decisions when selecting an insurance plan. The notice typically includes detailed information about the duration of the exclusion period, which can vary depending on the specific policy and insurance provider. Different Types of Salt Lake Utah General Notice of Preexisting Condition Exclusion: 1. Time-limited Exclusion: Under this type, the insurance company may impose a temporary exclusion period for preexisting conditions. During this period, any treatment related to the preexisting condition will not be covered by the policy. However, after the exclusion period ends, coverage for the preexisting condition may be granted. 2. Permanent Exclusion: In certain cases, insurance providers may enforce a permanent exclusion for preexisting conditions. This means that the policyholder will never receive coverage for the preexisting condition, regardless of the duration of their policy. 3. Modified Exclusion: Some policies may have modified exclusions, where coverage for a preexisting condition is provided after a shorter duration compared to the standard exclusion period. The modified exclusion aims to strike a balance between the insurance company's risk management and the policyholder's healthcare needs. It is important for individuals seeking health insurance to carefully read and understand the Salt Lake Utah General Notice of Preexisting Condition Exclusion before selecting a policy. This allows policyholders to anticipate limitations or potential gaps in coverage and make informed decisions about their healthcare needs. Seeking clarification from the insurance provider or consulting with a qualified insurance agent can help ensure that individuals comprehend the implications of the preexisting condition exclusion on their coverage.
Salt Lake Utah General Notice of Preexisting Condition Exclusion
Description
How to fill out Salt Lake Utah General Notice Of Preexisting Condition Exclusion?
Preparing legal paperwork can be burdensome. In addition, if you decide to ask an attorney to draft a commercial contract, documents for proprietorship transfer, pre-marital agreement, divorce paperwork, or the Salt Lake General Notice of Preexisting Condition Exclusion, it may cost you a fortune. So what is the most reasonable way to save time and money and draw up legitimate forms in total compliance with your state and local regulations? US Legal Forms is a great solution, whether you're searching for templates for your personal or business needs.
US Legal Forms is biggest online catalog of state-specific legal documents, providing users with the up-to-date and professionally verified forms for any use case gathered all in one place. Therefore, if you need the current version of the Salt Lake General Notice of Preexisting Condition Exclusion, you can easily locate it on our platform. Obtaining the papers takes a minimum of time. Those who already have an account should check their subscription to be valid, log in, and select the sample using the Download button. If you haven't subscribed yet, here's how you can get the Salt Lake General Notice of Preexisting Condition Exclusion:
- Glance through the page and verify there is a sample for your area.
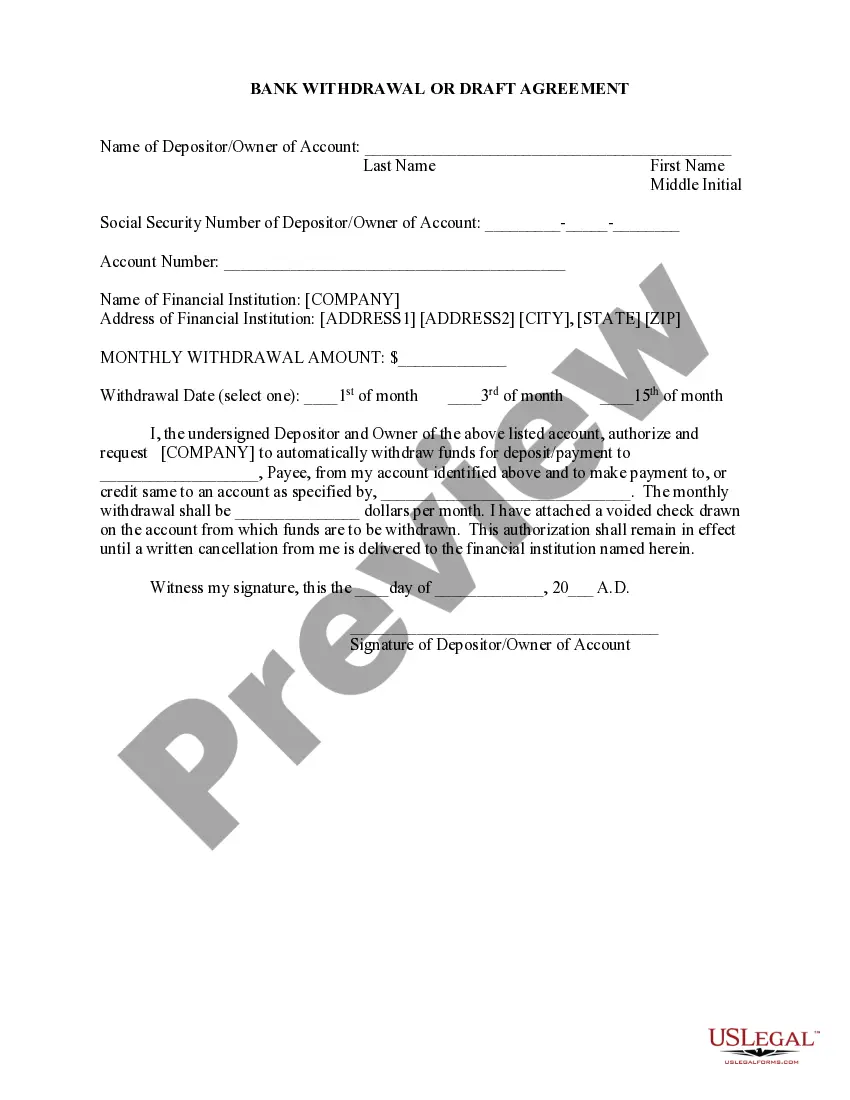
- Examine the form description and use the Preview option, if available, to make sure it's the template you need.
- Don't worry if the form doesn't suit your requirements - look for the correct one in the header.
- Click Buy Now when you find the needed sample and choose the best suitable subscription.
- Log in or register for an account to purchase your subscription.
- Make a payment with a credit card or via PayPal.
- Choose the file format for your Salt Lake General Notice of Preexisting Condition Exclusion and download it.
When finished, you can print it out and complete it on paper or upload the template to an online editor for a faster and more convenient fill-out. US Legal Forms allows you to use all the paperwork ever purchased many times - you can find your templates in the My Forms tab in your profile. Give it a try now!