San Antonio, Texas General Notice of Preexisting Condition Exclusion serves as an important document that outlines the terms and conditions regarding preexisting health conditions for individuals availing of certain insurance policies or healthcare plans within the San Antonio, Texas area. This notice helps ensure transparency and clarity in the insurance process while taking into account the existence of preexisting conditions. The San Antonio, Texas General Notice of Preexisting Condition Exclusion is typically applicable to various types of insurance coverage, such as health insurance, life insurance, disability insurance, and sometimes even employer-sponsored benefit plans. The purpose is to inform policyholders about any preexisting condition exclusions that may be applied to their coverage. Preexisting conditions are generally defined as health problems that an individual has been diagnosed with or treated for before obtaining the insurance policy or joining the specific healthcare plan. The inclusion of a preexisting condition exclusion allows insurance providers to mitigate risk and prevent potential abuse or fraud by individuals who may try to obtain coverage to address existing health conditions. It is important to note that the specific details and terms of the San Antonio, Texas General Notice of Preexisting Condition Exclusion may vary across insurance companies, plans, and policies. However, some common keywords and concepts may be found: 1. Definition of preexisting conditions: The notice will clearly outline what constitutes a preexisting condition, typically referring to any health issue for which an individual received medical advice, diagnosis, or treatment before their policy's effective date. 2. Waiting periods: Insurance companies often establish waiting periods during which preexisting conditions will not be covered. This means that any treatment or services related to these conditions will be excluded from coverage until the waiting period has passed. 3. Exceptions or limitations: The notice may describe certain exceptions or limitations to the preexisting condition exclusion. For example, coverage may be provided if certain conditions are met, such as continuous prior coverage without a significant gap. 4. Notification requirements: Policyholders may be required to notify the insurance company about any preexisting conditions within a specified timeframe after policy inception or enrollment. Failure to provide this information within the designated window may result in denial of coverage for related treatments. 5. Appeals process: If a claim is denied based on a preexisting condition exclusion, the notice will typically outline the steps policyholders can take to appeal the decision, ensuring a fair review process. The San Antonio, Texas General Notice of Preexisting Condition Exclusion is a crucial component of insurance policies and plans to ensure policyholders are informed about any limitations and exclusions that may apply. Being aware of this information can help individuals make informed decisions when choosing an insurance policy or healthcare plan in San Antonio, Texas.
San Antonio Texas General Notice of Preexisting Condition Exclusion
Description
How to fill out San Antonio Texas General Notice Of Preexisting Condition Exclusion?
A document routine always accompanies any legal activity you make. Opening a company, applying or accepting a job offer, transferring property, and many other life situations require you prepare formal documentation that differs from state to state. That's why having it all accumulated in one place is so helpful.
US Legal Forms is the most extensive online collection of up-to-date federal and state-specific legal templates. On this platform, you can easily locate and get a document for any individual or business objective utilized in your county, including the San Antonio General Notice of Preexisting Condition Exclusion.
Locating templates on the platform is extremely straightforward. If you already have a subscription to our service, log in to your account, find the sample using the search bar, and click Download to save it on your device. After that, the San Antonio General Notice of Preexisting Condition Exclusion will be accessible for further use in the My Forms tab of your profile.
If you are using US Legal Forms for the first time, adhere to this quick guideline to obtain the San Antonio General Notice of Preexisting Condition Exclusion:
- Make sure you have opened the correct page with your local form.
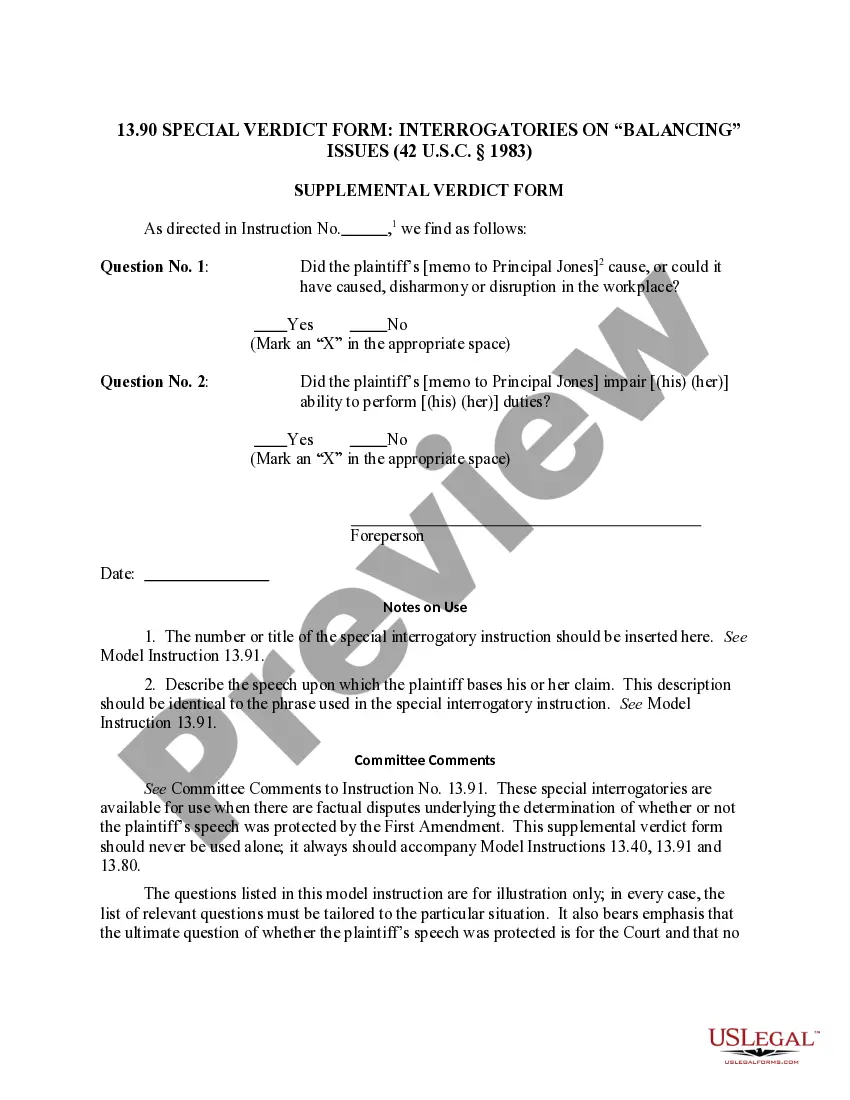
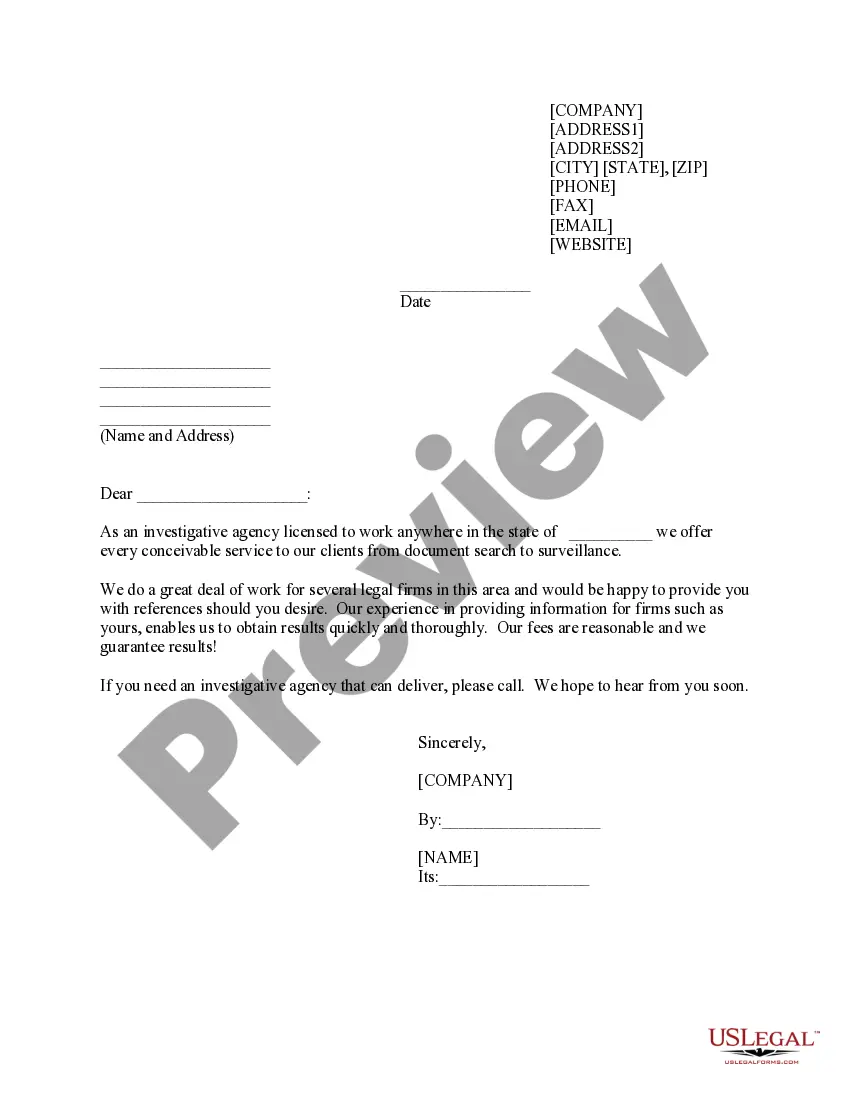
- Utilize the Preview mode (if available) and browse through the sample.
- Read the description (if any) to ensure the template meets your requirements.
- Look for another document using the search option if the sample doesn't fit you.
- Click Buy Now when you locate the necessary template.
- Select the appropriate subscription plan, then sign in or register for an account.
- Select the preferred payment method (with credit card or PayPal) to proceed.
- Choose file format and save the San Antonio General Notice of Preexisting Condition Exclusion on your device.
- Use it as needed: print it or fill it out electronically, sign it, and file where requested.
This is the simplest and most reliable way to obtain legal paperwork. All the samples available in our library are professionally drafted and checked for correspondence to local laws and regulations. Prepare your paperwork and manage your legal affairs efficiently with the US Legal Forms!