The Harris Texas Notice of Special Enrollment Rights is an important document that specifies the rights and options available to residents of Harris County, Texas, when it comes to enrolling in health insurance plans. This notice ensures that individuals are adequately informed about their opportunities for obtaining or changing their health coverage during specific enrollment periods. The Notice of Special Enrollment Rights outlines the various scenarios under which individuals may qualify for a special enrollment period. These situations can include losing previous coverage due to job loss, marriage, the birth or adoption of a child, or if a person becomes ineligible for Medicaid or Children's Health Insurance Program (CHIP) coverage. It also addresses the rights of individuals who were previously denied coverage for certain reasons, such as pre-existing conditions. By understanding the Harris Texas Notice of Special Enrollment Rights, residents gain knowledge about their rights to access health insurance coverage outside the regular open enrollment period. This information is particularly crucial for those who experience qualifying life events that enable them to seek coverage during special enrollment periods. Additionally, it is important to note that there may be different variations or types of the Harris Texas Notice of Special Enrollment Rights, depending on the specific health insurance programs available in Harris County. These variations may arise due to differences in eligibility criteria or program regulations. However, regardless of the specific name or type, these notices serve the same purpose of informing individuals about their special enrollment rights and the associated options available to them. In conclusion, the Harris Texas Notice of Special Enrollment Rights is a vital document that ensures residents understand their rights and options for obtaining or changing health insurance coverage during special enrollment periods. This knowledge empowers individuals and families to make informed decisions about their healthcare needs, especially in situations that lead to eligibility changes outside the regular open enrollment period.
Harris Texas Notice of Special Enrollment Rights
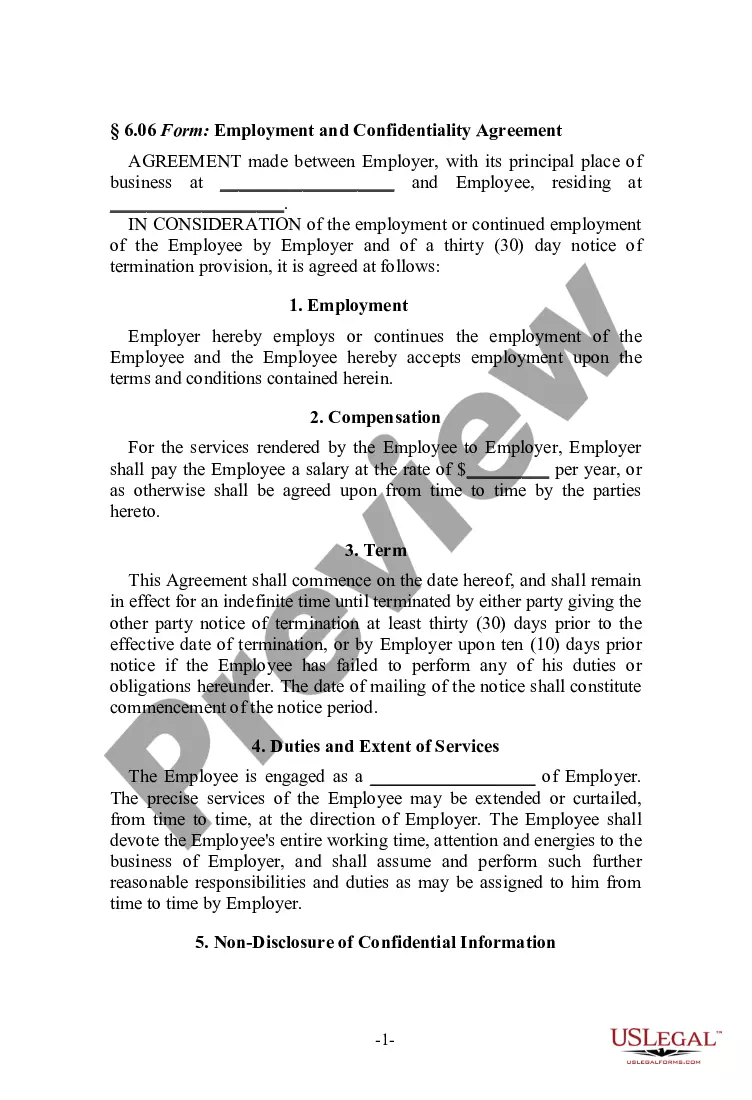
Description
How to fill out Harris Texas Notice Of Special Enrollment Rights?
Draftwing documents, like Harris Notice of Special Enrollment Rights, to manage your legal matters is a tough and time-consumming process. A lot of circumstances require an attorney’s involvement, which also makes this task expensive. However, you can consider your legal affairs into your own hands and take care of them yourself. US Legal Forms is here to save the day. Our website comes with over 85,000 legal forms intended for different cases and life situations. We ensure each form is in adherence with the regulations of each state, so you don’t have to worry about potential legal issues compliance-wise.
If you're already aware of our website and have a subscription with US, you know how easy it is to get the Harris Notice of Special Enrollment Rights form. Go ahead and log in to your account, download the template, and customize it to your needs. Have you lost your form? Don’t worry. You can find it in the My Forms folder in your account - on desktop or mobile.
The onboarding process of new users is fairly easy! Here’s what you need to do before downloading Harris Notice of Special Enrollment Rights:
- Ensure that your template is compliant with your state/county since the regulations for writing legal papers may differ from one state another.
- Find out more about the form by previewing it or going through a quick description. If the Harris Notice of Special Enrollment Rights isn’t something you were hoping to find, then take advantage of the search bar in the header to find another one.
- Sign in or create an account to begin utilizing our service and get the form.
- Everything looks great on your end? Hit the Buy now button and select the subscription option.
- Pick the payment gateway and type in your payment details.
- Your form is all set. You can try and download it.
It’s easy to find and buy the appropriate template with US Legal Forms. Thousands of organizations and individuals are already taking advantage of our rich collection. Subscribe to it now if you want to check what other benefits you can get with US Legal Forms!