Salt Lake City Utah Authorization Request for Medical Procedures/Carrier Response is a formal process in which healthcare providers seek approval from insurance carriers before performing certain medical procedures or treatments. This ensures that the requested procedure is medically necessary and covered by the patient's insurance policy. Here is a detailed description of this process, highlighting its importance and key elements: 1. Definition: An authorization request is a formal written documentation submitted by healthcare providers to insurance carriers for approval before performing specific medical procedures or treatments. It is essential to ensure proper communication and reimbursement between the provider, patient, and insurance company. 2. Purpose: The purpose of an authorization request is to obtain approval from the insurance carrier to proceed with a specific medical procedure or treatment. This is especially important for elective or costly procedures, as insurance companies may require additional information to determine if the procedure is medically necessary and covered under the patient's policy. 3. Submission Process: The healthcare provider initiates the authorization request by completing a form or submitting relevant documentation to the insurance carrier. This may include medical records, diagnostic test results, treatment plans, and other supporting documents. The request is typically sent through electronic means, such as secure online portals or fax, to ensure privacy and traceability. 4. Information Required: The authorization request should include crucial details about the patient, provider, and the requested procedure. This typically includes the patient's demographic information, medical history, diagnosis, and treatment plan. It is vital to provide accurate and complete information, as any missing or incorrect details could result in delayed or denied approval. 5. Different Types of Authorization Requests: In Salt Lake City, Utah, authorization requests for medical procedures may vary depending on the nature of the treatment or procedure. Common types of authorization requests include: a. Surgical Procedures: Requests for surgical procedures, such as major surgeries, organ transplants, or other invasive treatments, require detailed documentation to support the medical necessity and expected outcomes. These requests may involve collaboration between surgeons, specialists, and primary care physicians. b. Diagnostic Tests: Authorization for diagnostic tests, including radiological procedures (MRI, CT scan, X-rays), biopsies, or genetic testing, may also be required. The provider needs to provide clear clinical justification for the requested tests, explaining their relevance in diagnosing or monitoring the patient's condition. c. Specialty Care: Authorization requests for specialty care services, such as consultations with specialists or referrals to specific healthcare providers, might also be necessary. In such cases, providers need to describe the patient's condition and why the referral or consultation is essential for an accurate diagnosis or appropriate treatment plan. 6. Carrier Response: Upon receiving the authorization request, the insurance carrier reviews the provided information and evaluates its medical necessity and compliance with the patient's policy. The carrier's decision may take various forms, including: a. Approval: If the request meets the carrier's criteria and is deemed medically necessary, the carrier provides authorization to proceed with the requested medical procedure. The approval usually includes details regarding any pre-authorization requirements, such as specific providers, facilities, or other limitations. b. Denial: If the request does not meet the carrier's criteria or is considered not medically necessary, the carrier may deny the request. A denial can occur due to various reasons, such as lack of clinical justification, policy exclusions, or inadequate documentation. In case of denial, the provider can appeal the decision or explore alternative treatment options. c. Additional Information Requested: Sometimes, the carrier may request additional information or clarification to make a decision. In such cases, the provider needs to promptly provide the required details to ensure a prompt resolution. In conclusion, Salt Lake City Utah Authorization Request for Medical Procedures/Carrier Response is a crucial process that facilitates proper communication, documentation, and reimbursement between healthcare providers and insurance carriers. The different types of authorization requests mentioned above highlight its comprehensive nature, ensuring that medical procedures and treatments are medically necessary and covered by the patient's insurance policy.
Salt Lake City Utah Authorization Request for Medical Procedures/Carrier Response
Description
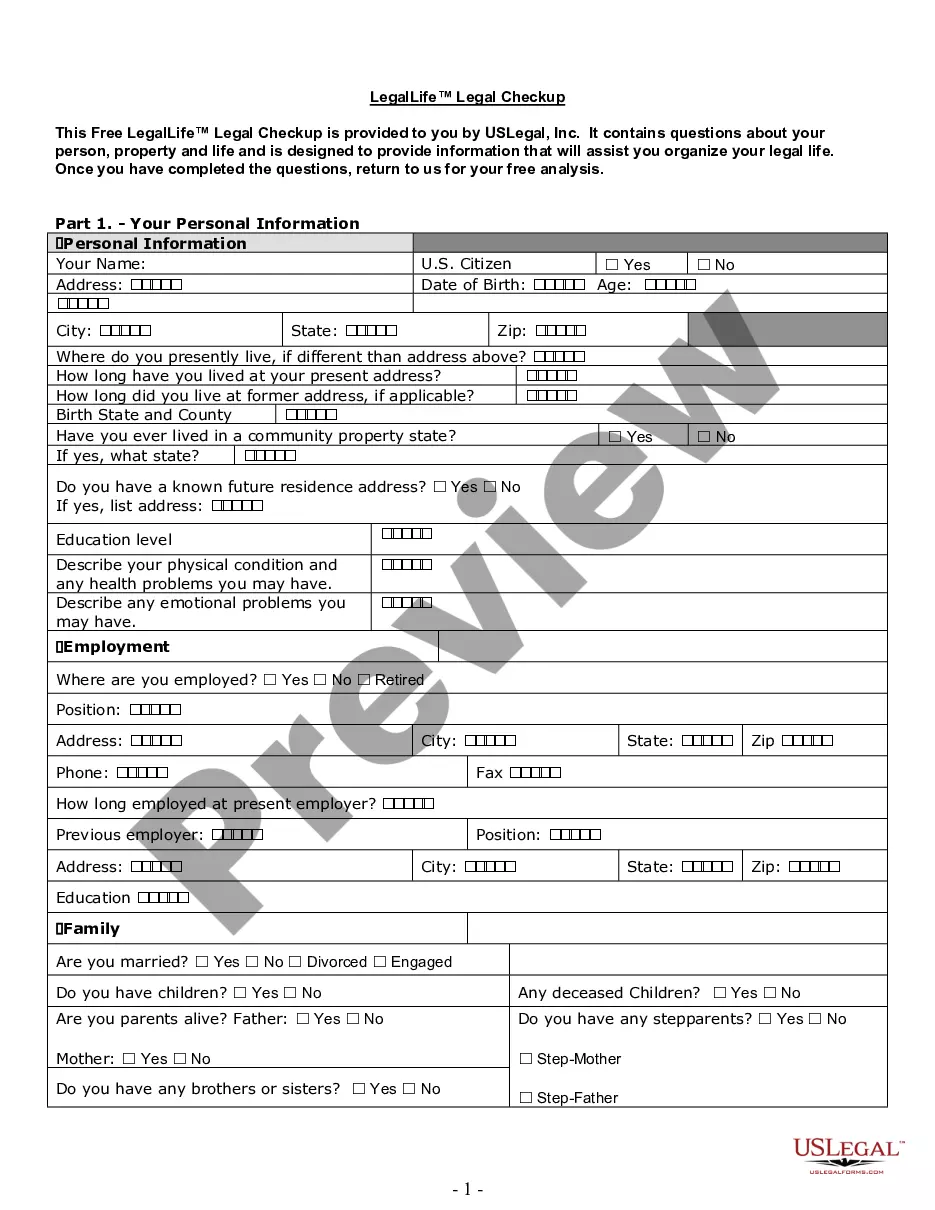
How to fill out Salt Lake City Utah Authorization Request For Medical Procedures/Carrier Response?
No matter the social or professional status, filling out legal documents is an unfortunate necessity in today’s professional environment. Too often, it’s practically impossible for a person without any law education to draft such papers from scratch, mainly due to the convoluted terminology and legal subtleties they involve. This is where US Legal Forms comes in handy. Our platform provides a massive collection with over 85,000 ready-to-use state-specific documents that work for almost any legal situation. US Legal Forms also is a great resource for associates or legal counsels who want to save time utilizing our DYI forms.
Whether you need the Salt Lake City Utah Authorization Request for Medical Procedures/Carrier Response or any other document that will be good in your state or area, with US Legal Forms, everything is on hand. Here’s how you can get the Salt Lake City Utah Authorization Request for Medical Procedures/Carrier Response quickly employing our trusted platform. If you are already an existing customer, you can go on and log in to your account to download the needed form.
Nevertheless, if you are a novice to our library, make sure to follow these steps prior to obtaining the Salt Lake City Utah Authorization Request for Medical Procedures/Carrier Response:
- Be sure the form you have found is specific to your area since the regulations of one state or area do not work for another state or area.
- Preview the document and read a brief description (if available) of cases the paper can be used for.
- If the form you chosen doesn’t meet your needs, you can start over and look for the needed form.
- Click Buy now and choose the subscription option you prefer the best.
- with your credentials or create one from scratch.
- Choose the payment method and proceed to download the Salt Lake City Utah Authorization Request for Medical Procedures/Carrier Response once the payment is completed.
You’re good to go! Now you can go on and print the document or complete it online. If you have any issues getting your purchased documents, you can quickly find them in the My Forms tab.
Whatever case you’re trying to sort out, US Legal Forms has got you covered. Try it out now and see for yourself.