Title: Provo Utah Notice to Medicaid Recipient — Understanding the Various Types and Importance Introduction: The Provo Utah Notice to Medicaid Recipient is a crucial document that serves as a direct communication channel between the Medicaid program and its recipients in the Provo, Utah area. This notice conveys important information regarding eligibility, benefits, changes in coverage, and other significant updates that recipients must be aware of. In this article, we will explore the different types of Provo Utah Notice to Medicaid Recipient and highlight the vital keywords associated with each type. 1. Types of Provo Utah Notice to Medicaid Recipient: a. Eligibility Notice: The Eligibility Notice is one of the key types of notices that Medicaid recipients in Provo, Utah receive. It provides detailed information about an individual's eligibility status, including any changes, renewal deadlines, and requirements to maintain coverage. b. Benefit Change Notice: This type of notice is sent to Medicaid recipients in Provo, Utah to notify them about any changes in their benefits, such as modifications in coverage, co-payment adjustments, or alterations in the services covered by the Medicaid program. It clarifies the impact of such changes and offers guidance on adapting to the new benefits structure. c. Managed Care Enrollment Notice: In the event of Provo, Utah's Medicaid program implementing managed care, recipients will receive this notice. It informs them about their enrollment in a managed care organization, the organization's name, contact details, and relevant information on how to access healthcare services through the chosen managed care plan. d. Renewal Notice: The Renewal Notice is sent to Medicaid recipients within Provo, Utah, prompting them to renew their existing coverage before the expiration date. It outlines the necessary steps, documentation, and timelines for the renewal process, encouraging recipients to ensure their continuous eligibility for Medicaid benefits. e. Suspension/Termination Notice: If there are instances where a Medicaid recipient's coverage is at risk of suspension or termination due to non-compliance with program requirements, a notice is sent to provide fair warning. This notice entails the reasons, effective dates, and potential consequences of the suspension or termination, as well as instructions for appealing the decision or exploring alternative options. Conclusion: The Provo Utah Notice to Medicaid Recipient plays a crucial role in keeping Medicaid recipients within Provo, Utah well-informed about their eligibility, benefits, changes, and responsibilities under the Medicaid program. By familiarizing themselves with the different types of notices and paying close attention to their contents, recipients can ensure they make informed decisions and take necessary actions to maintain their Medicaid coverage effectively.
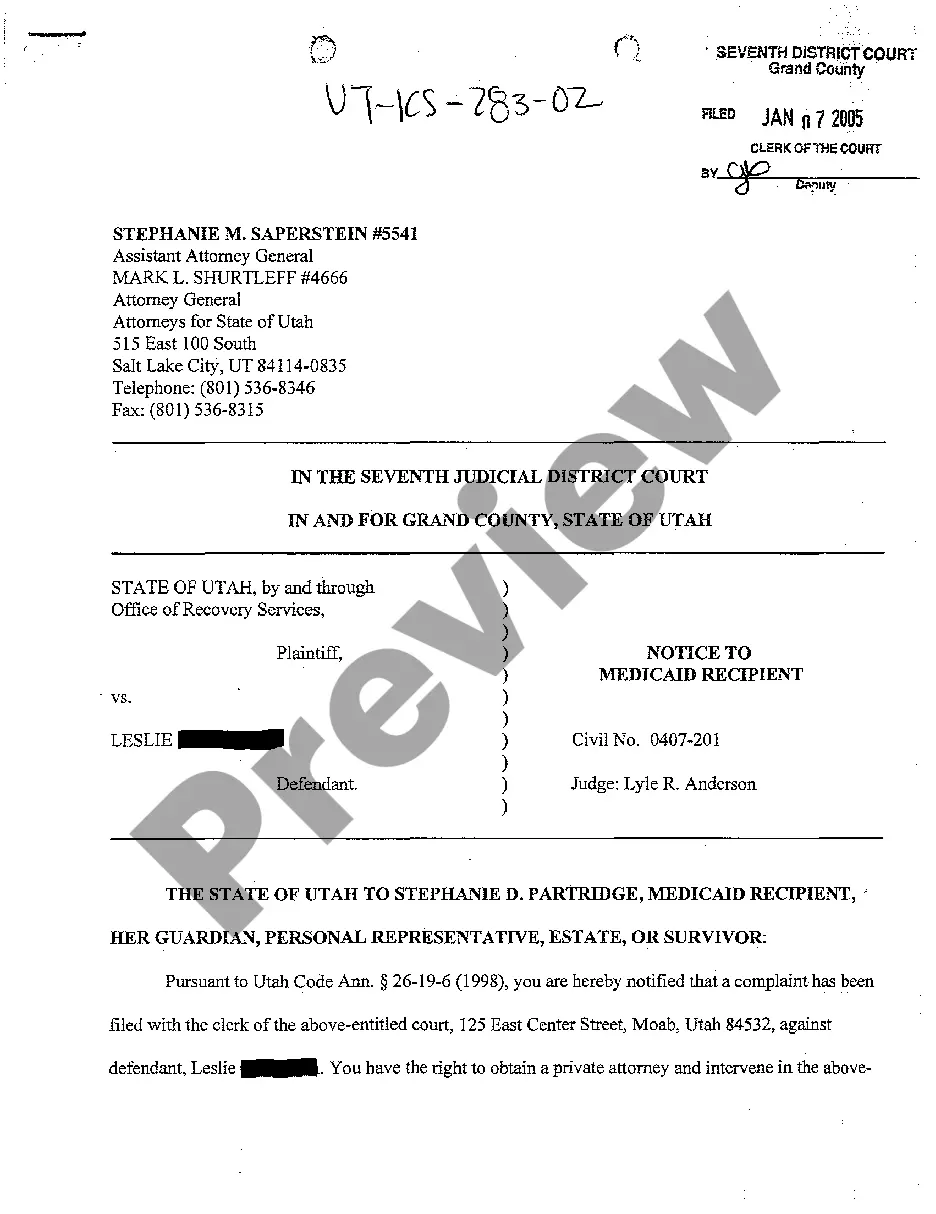
Provo Utah Notice To Medicaid Recipient
Description
How to fill out Provo Utah Notice To Medicaid Recipient?
Locating verified templates specific to your local laws can be difficult unless you use the US Legal Forms library. It’s an online collection of more than 85,000 legal forms for both personal and professional needs and any real-life situations. All the documents are properly grouped by area of usage and jurisdiction areas, so locating the Provo Utah Notice To Medicaid Recipient gets as quick and easy as ABC.
For everyone already acquainted with our library and has used it before, obtaining the Provo Utah Notice To Medicaid Recipient takes just a couple of clicks. All you need to do is log in to your account, select the document, and click Download to save it on your device. This process will take just a couple of more steps to complete for new users.
Adhere to the guidelines below to get started with the most extensive online form library:
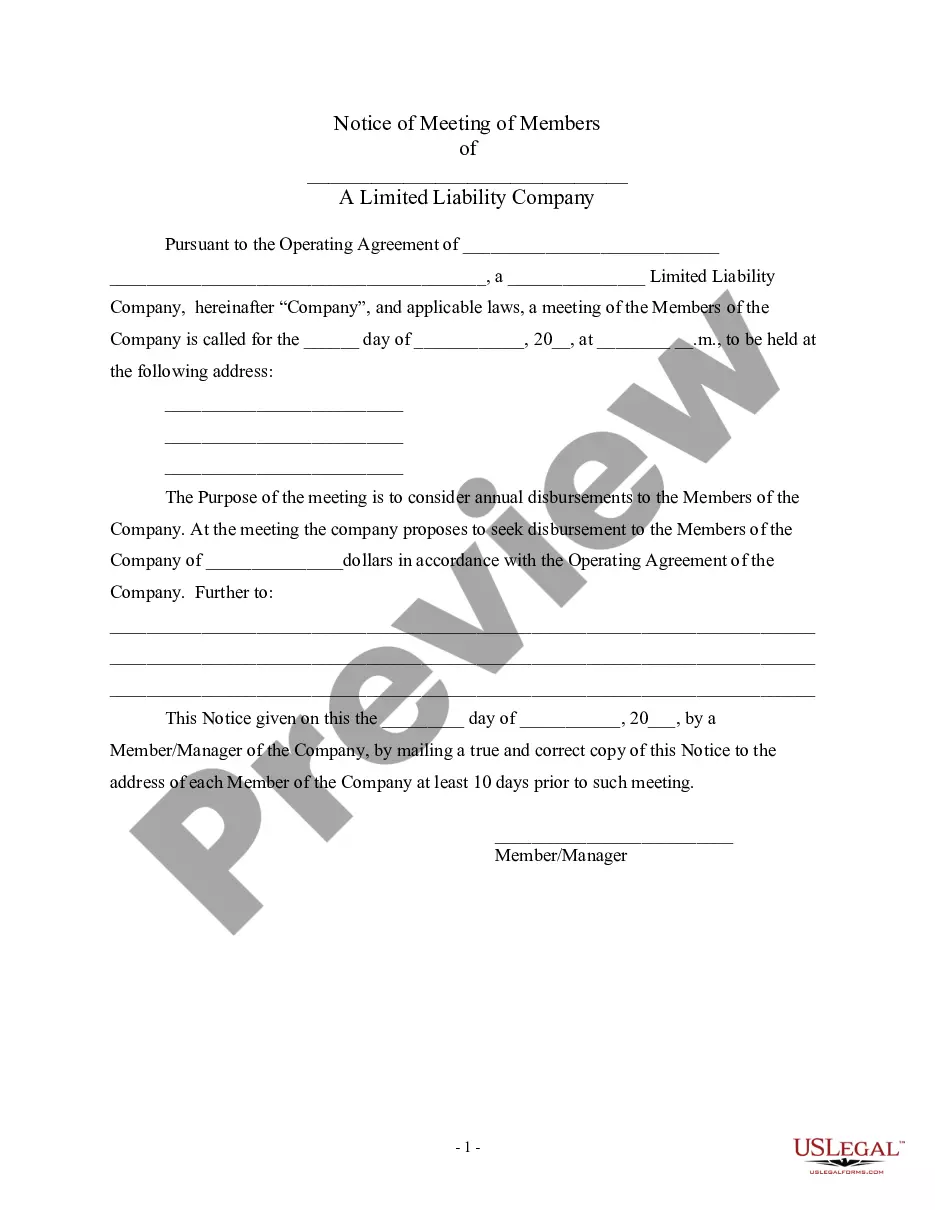
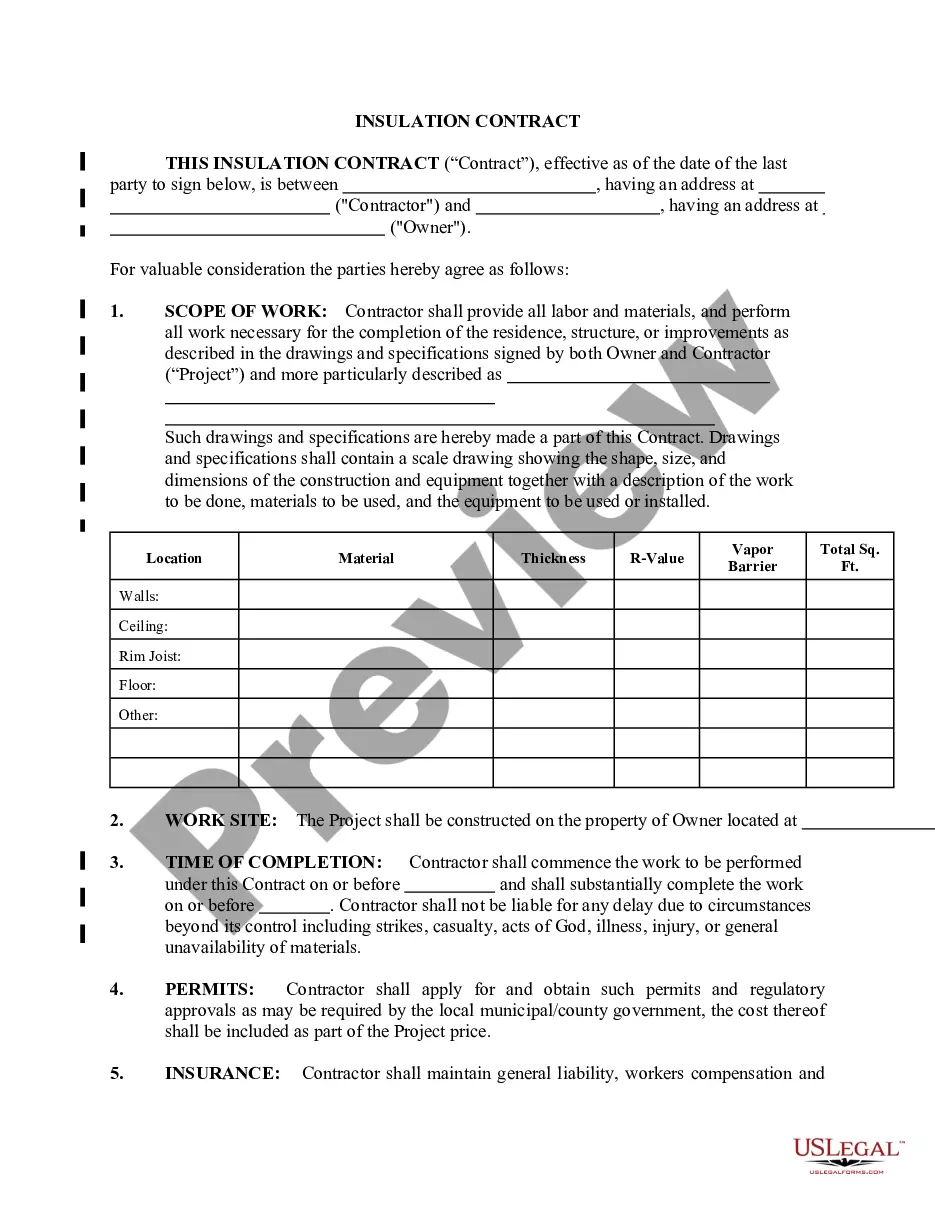
- Check the Preview mode and form description. Make certain you’ve picked the correct one that meets your requirements and fully corresponds to your local jurisdiction requirements.
- Search for another template, if needed. Once you find any inconsistency, utilize the Search tab above to get the correct one. If it suits you, move to the next step.
- Buy the document. Click on the Buy Now button and select the subscription plan you prefer. You should create an account to get access to the library’s resources.
- Make your purchase. Give your credit card details or use your PayPal account to pay for the subscription.
- Download the Provo Utah Notice To Medicaid Recipient. Save the template on your device to proceed with its completion and obtain access to it in the My Forms menu of your profile anytime you need it again.
Keeping paperwork neat and compliant with the law requirements has significant importance. Take advantage of the US Legal Forms library to always have essential document templates for any demands just at your hand!